Journal of
eISSN: 2373-6445


Research Article Volume 13 Issue 2
University of Nicosia, Cyprus
Correspondence: Yubaraj Adhikari, PhD, Department of Social Sciences, University of Nicosia, Cyprus
Received: September 01, 2022 | Published: September 21, 2022
Citation: Adhikari Y, Senft B. Distressed but Highly Satisfied: Professional and Personal Distress of Nepali Doctors. J Psychol Clin Psychiatry. 2022;13(2):41-55. DOI: 10.15406/jpcpy.2022.13.00713
Background: This research studied the prevalence of professional and personal distress of Nepali doctors, and examined the impact of their professional quality of life (ProQOL) on their distress.
Aim: To examine the situation of personal and professional distress and explore interrelationships between measures of ProQOL (burnout - BO, secondary traumatic stress - STS, and compassion satisfaction - CS) with personal distress (anxiety, depression and somatic burden) of Nepali doctors.
Methods: A survey design was used to examine the personal and professional distress of doctors using an online and a paper-and-pencil survey with the use of Somatic Symptoms Scale (SSS-8), Hopkins Symptoms Checklist (HSCL-25) and Professional Quality of life Scale in Nepali (ProQOL5-N) tools. Confirmatory factor analysis (CFA) and structural equation modeling (SEM) techniques were used to measure the influence of professional distress on personal distress.
Results: The prevalence of anxiety, depression, psychosomatic distress and suicide risks of Nepali doctors (N= 557) were 30.89 %, 25.41 %, 20.50% and 5.70% respectively. BO and STS scores showed moderate risks (BO = 95.25% and STS = 76.23 %), with just over 1% doctors at high risk for BO and STS (1.28% and 1.65% respectively). Nepali doctors were highly satisfied with their service (CS = 93.42%). The data on SEM showed a reasonably good fit between the STS and CS measures and levels of personal distress of the studied population, but BO could not be tested. A moderate but statistically significant positive effect of STS on personal distress, except psychosomatic distress, was found. The effect of CS on personal distress could not be determined.
Conclusions: One-fifth of Nepali doctors had a high level of personal distress. The risk for BO and STS was moderate. It was found that Nepali doctors found highly satisfied with their service. The impact of professional distress on personal distress could not be fully determined.
Keywords: Depression, Suicide, Burnout, ProQOL, SEM, Nepali Doctors
Background
Medical doctors are trained to be ‘passionate about medicine and compassionate about people. Being competent in practice and showing empathy to clients is not always an easy job. Doctors face constant emotional challenges too. The potential to derive self-satisfaction from the obligation to provide great can easily be jeopardized due to the inability to cope with the distress associated with providing care. Scientific studies conducted over the last two decades have reported high, even epidemic levels of career dissatisfaction, burnout (BO), secondary traumatization, depression, and suicide.1-5 ‘Burnout in physicians is common, and studies show a prevalence of 30% to 78% of compassion fatigue.’2 Depression and suicide among medical doctors are increasing, and statistics often show that they exhibit such manifestations of distress in greater proportions than the general population.
BO and STS are often related to the professional environment, whereas psychological distress such as depression, anxiety, and suicidal intent can be caused by broader ecological factors. The interrelationships of these variables differ depending upon organizational values, socio-cultural and economic contexts which cannot be generalized.6,7 Prolonged stress, secondary trauma, and BO aggravate the feelings of isolation, helplessness, and hopelessness medical doctors’ experience.
Untreated depression is the major cause of suicide.8 Male doctors have 1.41 times the suicide rate of the general population and female doctors, 2.27.9 Often, the natural mortality rate of doctors is lower than that of the general population, making the high deliberate self-harm rates particularly alarming. The negative effects of providing care among physicians have forced early retirements, resulted in non-clinical careers, and increased the practice of concierge medicine to limit the workload.5,10 A review of 72 published articles found that medical doctors often reported experiencing work-related stress, BO, and CF due to lack of job satisfaction, challenges in managing clinical cases, managerial issues, and poor working conditions.11 The news of medical doctors’ suicides, the stigma associated with seeking mental health support, and the fear of losing one’s license to practice have cast a pall over the medical profession.12
In developed countries, studies have shown that doctors report a higher level of distress than does the general population.13,14 The prevalence of depression, for example, is 15% to 30% higher among medical doctors than the general population.1 A systematic review of the literature on the depression and depressive symptoms of medical doctors, covering over 50 studies (n=17,560) since 1963, found that the average prevalence rate of depression was 28.8% and that this rate had increased every year.15 In the United States alone, 300-400 medical doctors commit suicide every year.8 In Australia, 1 out of 10 medical doctors and medical students with depression commit suicide.16 Studies from the United Kingdom, Denmark, and Canada also show that medical doctors are among the professional groups with the highest rates of depression.17-19
In Asia, a few studies have shown that nearly two-thirds of Chinese doctors are depressed.20,21 In Pakistan, one-third (34%, n = 203) of doctors were diagnosed with mild to moderate levels of anxiety and depression, and 1% were severely depressed.22 Nepal has a few studies on the mental health of medical students. The prevalence of anxiety was 41.1% (n = 538) and that of depression, 29.9%.23 In another study, 29.78% (n = 50) of medical undergraduate degree students were diagnosed with moderate and severe depression.24
A growing body of literature is presenting associations and interlinkages between professional and personal distress among medical professionals.25,26 Brenninkmeyer, Van Yperen, and Buunk27 reviewed the literature and concluded ‘depression and burnout seem closely related, but they are certainly not identical twins' (p. 879).’ Pompili et al.28 claimed BO is associated with depression and suicide. BO has also been found to correlate with perceived stress.29 McManus, Winder, & Gordon30 outlined the causal link between BO and stress.
The interrelationships among the factors of ProQOL (BO, STS, and CS) with personalized distress (anxiety, depression, and psychosomatic burden) are understudied or unpublished due to non-findings. Despite the growing interest in the professional and personal quality of life of medical doctors in Nepal,31 no nationwide study on the prevalence of distress and the state of the ProQOL of medical doctors in Nepal exists. This study also provides interrelationships between the measures of professional distress factors (ProQOL) and measures of personal distress (anxiety, depression, and psychosomatic burden).
As previous data and research on the prevalence of anxiety, depression, psychosomatic burden, BO, STS, and CS in the population of Nepali doctors was not available, a cross-sectional survey design was applied. The Nepal Medical Council (NMC) of registered doctors was considered as the universe and each doctor as a unit of the study. The Nepal Medical Council (NMC) had registered 15,479 medical doctors and 1,786 dental doctors by December 2015.32 Many medical doctors migrate; in fact, nearly 50% of new graduates and young doctors are either in the process of migrating to other countries or have already left. Out of the approximately, 10,000 doctors who are available in the country, over 40% are centralized in the capital city.33 Most medical doctors work in the private sector, and those associated with the government system also have private practices. Teaching hospitals, both government and private, are another sector where doctors are engaged. To a more limited extent, doctors are also involved in the non-profit sector.
To calculate sample size, Aday and Cornelius34 recommend applying n = Z21-α/2 X P (1-P)/d2, where the sample size is chosen based on the estimated population (P) and level of desired precision (d). A total sample size of 384 was calculated, using 95% as the confidence interval, 50% of the true population and a 5% marginal error. Hulley, Cummings, Browner, Grady, & Newman35 outline the use of n = [(Zα+Zβ)/C]2 + 3 to calculate the sample size in a correlational study. A total sample size of 194 was calculated, in which α = 0.05, power (1-β) = 0.8, and the expected correlation coefficient r = 0.20.35 Therefore, a sample size of 384 was determined to be sufficient to measure the correlation between the ProQOL and psychological distress among Nepali doctors. The sample size was calculated through using http://www.sample-size.net/correlation-sample-size/.36
All medical doctors, both male and female, who were registered with the NMC and over the age of 18, irrespective of the nature of their work or location of their job, were included in the study. Respondents below the age of 18 who declared themselves as well as those who were absent from medical practice due to mental illness or retirement were excluded. Students pursuing an undergraduate degree in medical science without having passed the NMC’s registration were also excluded. The data was collected from July 2018 to November 2018. This study concluded in April 2020.
The overall aim of this study was to measure ProQOL factors and psychological distress (anxiety, depression and psychosomatic problems) of Nepali medical doctors. Furthermore, the study also examined the level of influence ProQOL measures (BO, STS, and CS) have on anxiety, depression and psychosomatic problems in that same population.
Procedures
The data collection process primarily relied on the direct responses of respondents through an online process created with Google Docs. As some of the potential participants asked the researcher to approach them personally and collect data using a paper-and-pencil format, the researcher trained two research assistants, each with a master’s degree in social work and deployed them to collect the information. Research announcement emails were also sent to over fifty medical institutions to notify the medical doctors. The researcher shared the announcement of this research in various self-help platforms of Nepali doctors such as the Non-Governmental Doctors’ Association, Governmental Doctors’ Association, Doctors and Medical Society of Nepal, Doctors’ Society of Nepal, Doctor Story Nepal, Mental Health Concerns of Nepali Doctors, and Nepal Doctors’ Medical Society Consultants. The researcher also received a roster of the emails of cardiac, orthopedic and dental doctors, whom he then approached through a group email. In addition, 250 paper-and-pencil questionnaires together with the research announcement form, participant’s information sheet, and consent form were handed over to doctors with the support of the two research assistants.
For online responders, the research announcement, consent form, and questionnaire were consolidated in one document so that respondents would get the package at once. The questionnaire package, which included Nepali Version of Professional Quality of Life 5(N-ProQOL-5), Nepali version of Hopkins Symptoms Checklist (HSCL-25), Somatic Symptom Scale (SSS – 8), and socio-demographic information was prepared in both paper and online forms. Providing data would have taken a respondent approximately 30-35 minutes. At any point of time in the process, the respondent had the right to withdraw without providing an explanation. It was very difficult to track the response rate to the online announcement. The researcher received 400 online responses. Out of the 250 paper questionnaires distributed, 147 questionnaires were returned, making the response rate 59%. In the process of data collection, all the respondents were provided with a debriefing letter, which included a thank you note, information on services available for therapeutic and counseling support and the contact details of the researcher if the respondent wished to contact for any advice or for a summary of the findings of the research.
Demographic data
Consent and demographic data were gathered in English, but responses to ProQOL and personal distress were asked in Nepali. At the end of the survey, respondents were asked to fill in some demographic and work-related responses. The demographic information collected includes gender, age, qualification, and type of institution at which the respondent works. They were also requested to indicate years of experience, place of work, any self-care training and availability of clinical supervision.
Nepali Version of Professional Quality of Life 5
ProQOL-5 consists of 30 items in all, 10 each for CS, BO, and STS. Each item is scored on a scale of five, the Likert scale, where 1=Never, 2= Rarely, 3=Sometimes, 4=Often, and 5=Very Often. Stamm37 stated that the cut-off scores for each sub-scale fall below the 25th or above the 75th percentiles. Sodeke-Gregson et al.38 found that each sub-scale of ProQOL-5 has a good internal consistency reliability (CS α=0.88 [n=1,130]; BO α=0.75 [n=976]; CF α=0.81 [n=1,135]). According to Stamm,37 the ProQOL-5 has been translated, contextualised, used and validated in more than a dozen languages. The researcher translated, used and contextualised a Nepali version of ProQOL5, namely N-ProQOL-5.39 The Pearson correlation in N-ProQOL-5 (n =112) was explored and found that STS and CS as well as BO and CS are significantly but negatively correlated with r = -.197, p = .05 and r = -.689, p <0.001 respectively. A positive correlation was observed between BO and STS with r = 0.614, p <.001. The overall reliability was modest with a reliability coefficient of 0.651.39 N-ProQOL-5 was reviewed and accepted by the ProQOL governing institution, the Center for Victims of Torture (CVT), after the creator of ProQOL, Dr. Beth HudnallStamm, had retired.
Nepali version of Hopkins Symptoms Checklist (HSCL-25)
HSCL-25 covers the symptoms of anxiety and depression and comprises 25 items. The first 10 items of the scale measure symptoms of anxiety and the next 15 items measure the symptoms of depression including 1 item measuring suicidal ideation. Respondents had to choose one out of four categories, “Not at all,” “A little,” “A lot,” and “Extremely,” which are rated 1 to 4 respectively. The internal consistency of these measures is high, and the reliability coefficient Cronbach α was measured to be from 0.84 to 0.87.40,41 Thapa and Hauff41 applied HSCL-25 to the Nepali population. The reliability coefficient (Cronbach α) they found for anxiety and depression was 0.89, and both the anxiety and depression scales had a cut-off score of 1.75.
Nepali version of Somatic Symptom Scale (N-SSS – 8)
SS-8 covers an individual’s somatic symptoms burden. It has eight self-reported items ranked on a 5-point Likert scale (0 = Not at all, 1 = A little bit, 2 = Somewhat, 3 = Quite a bit, and 4 = Very much). SSS-8 has good reliability as measured with Cronbach α (α = 0.81) good internal consistency.42 The construct validity of the SSS-8 showed a positive correlation between SSS, and the symptoms of both anxiety and depression. Tests of the confirmatory factorial analysis (CFA) confirmed that somatic symptoms lie in four clusters: gastrointestinal, pain, cardiopulmonary and fatigue related factors.42 The content validity of SSS-8 is good. It includes, as recommended by Zijlema et al.43 cardiopulmonary-related symptoms while measuring somatic symptoms. SSS-8 was adapted culturally and translated into Nepali, both forward-backward translations, with appropriate pilot testing before it was used in the final data collection process.
Data Analysis Process
The data analysis process included data entry, coding, and cleaning. The online data were downloaded from the data repository where the responses from the participants were automatically restored. As SSS-8 was translated into Nepali and tested in the Nepali population for the first time, a pilot study to verify the reliability and validity of the tool was conducted. For this purpose, the first 55 responses were used as pilot sample data. The data was checked for missing values. None were found. Appropriate coding, tabulation, and analysis were carried out. The psychometrics and model fit on the CFA of the tool together with the scores on validity and reliability were satisfactory, so the full study was launched. The results are presented in the results section.
The online data collection portal provided automated responses from 400 respondents. The data received in physical form (n = 157) were individually typed into a similar format and merged with the online data. The refined data of 557 respondents was copied in SPSS-25 student version, and appropriate variables were coded. No missing data were found in the online repository. SPSS worksheet data were verified for anomalies and cleaned. The few missing data on the physical forms were explored and treated by putting in the mean value of the items. Normality, homogeneity of the variances, linearity and multicollinearity, and co-variances were tested before a detailed analysis was performed. Apart from the correlations among the variables, Levene’s test for the homogeneity of variances was also conducted.
Descriptive statistical analysis was applied to measure the means and standard deviations of continuous variables. The significant testing for normality followed the distribution checks via scatterplots, box plots, kurtosis, and skewness. A Pearson's product-moment correlation was analysed after testing the relevant assumptions for the correlation. Field44 analyzed and suggested that Kolmogorov Smirnov and Shapiro-Wilk test results are only accurate for the smaller sample size studies. In large samples, the researcher has to analyze the normality based on the visual inspection of histograms, Q-Q plots, box plots, and interpretation of skewness and kurtosis scores. Histograms, normal Q-Q plots, box plots, scatter plots, Mahalanobis’ distances for the DVs and residuals were reviewed. The skewness and kurtosis were tested for all the items of both the anxiety and depression measures. The kurtosis values of depression were found slightly positively deviated. The quadratic Mahalanobis’ distance (MD2) was used to outline possible outliers. Some outliers were identified, but there were no major differences even after they were deleted. Therefore, the normality of the data was ensured.
The cumulative scores on the subscales of ProQOL (BO, STS and CS) of the participants were used as independent variables (one at a time) while scores for anxiety, depression and somatic problems were considered as dependent variables. The prevalence of BO, STS, CS, anxiety, depression and somatic problems were outlined.
Then, a path analysis diagram was drawn into the AMOS by using individual items of the measures. The interlinkages among the variables were prepared. SPSS AMOS- 25 version was used for data analysis. To investigate the factor loadings and structures of each measure of ProQOL (psychosomatic, anxiety and depression measures) in the new data set of 547 respondents, a path analysis diagram for each measure was drawn into AMOS using individual items of the measures. CFAs of SSS-8, ProQOL-5, and HSCL-25 were carried out. Several model fit indices and fit criteria such as chi-square, goodness-of-fit index (GFI), adjusted goodness-of-fit index (AGFI), normed fit index (NFI), Tucker-Lewis Index (TLI), comparative fit index (CFI), and root mean square error of approximation (RMSEA) to examine the goodness of fit of the CFA model of SSS-8, ProQOL-5 and HSCL-25 measures were applied. After the model fit examination, construct reliability (CR) for convergent validity and average variance extracted (AVE) for discriminant validity were analysed for further use of the tools.
In the SEM, there is no consensus about which fit indices are to be analysed and presented to define whether or not the tested model is absolutely fit. Instead, there are various fitness indexes to determine if the model is the best fit with the given data.45,46 It is recommended that three commonly agree upon standardised fitness indices (absolute fit indices, incremental fit indices, and parsimonious fit indices) be reported on.45-48 After analysing various peer-reviewed resources, Ahmad, Zulkurnain, and Khairushalimi49 consolidated standardised fitness indices. These were applied to consider the best fit of the model.
Last, the items with the best model fit for each measure were taken for further analysis. A structural model comprising measures of SSS-8, ProQOL-5 and HSCL-25 was drawn. The interlinkages among the variables were prepared. A SEM was applied to understand associations and relationships among the factors of ProQOL and distress. Explicitly, a positive association between the depression, anxiety and psychosomatic scores of Nepali medical doctors and their scores of BO and STS was checked. Inversely, the measures of CS should have a negative correlation with anxiety, depression and psychosomatic symptoms, a hypothesis which was tested. The final model fit indices and diagram with necessary details were tested with the aim and objective of this study.
The researcher followed the ethical approval process of the research ethics committee of the Austrian Academy of Psychology (AAP), which was that assigned and accepted by the university of Nicosia. In addition, the researcher received a local ethics approval from the National Health Research Council (NHRC), Kathmandu. Both ethical clearances were granted before the start of the data collection process in July 2018. The researcher provided the research announcement letter and participants’ information sheet to prospective participants through an online and anonymous data collection process. All participants were requested to read the participant information sheet, which explained that participation was voluntary and that they could withdraw from participation at any time without providing a justification. Prospective respondents who received a sealed envelope were not forced to return it and were never asked why they had not done so. As a result, only 147 out of 250 envelopes were returned.
Respondents were not asked for personal information such as their names, emails or phone numbers, an omission which respected their privacy. The contact details of the researcher and two providers of mental health and counseling support services were provided in a debriefing later if the respondents wanted a consultation. Before the data collection process started, approval for the referral to services was granted from Transcultural Psychosocial Organisation Nepal and Rhythm Neuropsychiatry Hospital and Research Center private limited. The physical data and the consent form for the pencil-and-paper responses were separated from the data entry process. Since, no personal data which may identify the responses of any respondent were entered or processed, the anonymity, privacy, and confidentiality of the respondents were well respected in all the steps of this research.
Socio-demographic information of the respondents
Out of the 557 responses, male and female responses were 415 (75.90 %) and 129 (23.60 %) respectively. Three respondents (0.5%) recorded no gender option. The socio-demographic data reveals that over half of the respondents (55.39 %) had a home-based job and 44.61% were working in out-of-home locations. One out of two doctors (52.83 %) were from Kathmandu Valley, 6.22% of the doctors participated from abroad, and 40.95 % were serving out of the capital. The participation of doctors working in government hospitals was encouraging: 242 doctors (44.24%) reported that they do so. Altogether 175 doctors (31.99 %) doctors were associated with private hospitals and 97 doctors (17.73 %) worked at teaching hospitals. Small numbers worked in private practices or non-governmental (public) hospitals, just 3.66% and 2.38% respectively. The dominant age group, with 451 respondents (82.45%), was 26–45 years of age, but 12.25% of doctors were below 25 years of age and 4.75% (26 doctors) were over 46. Just three were older than 60. Of the participants, 52.3% were medical doctors and 28% general practitioners or consultant doctors. Senior consultants and directors constituted 7.1 % and 1.6 % of the respondents respectively. In addition, there were 55 resident doctors (10.10 %). Interestingly, only one out of three doctors (30.90 %) received clinical supervision, 11.3% of participants had never heard of it, and 57.77 % of doctors were working without clinical supervision. Only 5.48 % of doctors had participated in self-care or care-for-care-providers workshops and training in the last one-year period. About 36.5 % of the respondents had a master’s degree and 11% had a doctorate degree in medicine. The socio-demographic details are given in Table 1 below.
Characteristics |
Sub-Heading |
N |
Percentage |
Gender |
Male |
415 |
75.9 |
Female |
129 |
23.6 |
|
Unknown |
3 |
0.5 |
|
Position |
General physician / Dental doctor |
291 |
53.2 |
Consultant |
153 |
28 |
|
Senior Consultant |
39 |
7.1 |
|
Director |
9 |
1.6 |
|
Resident Doctor |
55 |
10.1 |
|
Qualification |
Bachelor of Medicine/Dental |
288 |
52.7 |
Master’s in Medicine/Dental |
199 |
36.3 |
|
Doctorate in Medicine |
60 |
11 |
|
Experience |
0-2 Years |
188 |
34.4 |
> 2-5 Years |
183 |
33.46 |
|
> 5-10 Years |
109 |
19.93 |
|
> 10+ Years |
67 |
11.88 |
|
Type of Institution |
Government Hospital |
242 |
44.24 |
Private Hospital |
175 |
31.99 |
|
Teaching Hospital |
97 |
17.73 |
|
Private Practice |
20 |
3.66 |
|
Non-Governmental/Public |
13 |
2.38 |
|
Type of Service |
Emergency Service |
97 |
17.73 |
Out-Patient |
36 |
6.58 |
|
Surgery or Post-Operative |
225 |
41.13 |
|
Clients at Private Clinic |
89 |
16.27 |
|
Other (not mentioned above) |
74 |
13.53 |
|
All of the Above |
26 |
4.8 |
|
Caseload per Week |
Below 25 |
124 |
22.67 |
26-49 |
153 |
27.97 |
|
50-75 |
120 |
21.94 |
|
|
76 or above |
150 |
27.42 |
Table 1 Socio-Demographic Details of the Respondents
Prevalence of distress among nepali medical doctors
The Cronbach alpha for anxiety, depression and psychosomatic disorders were .890, .926, and .802 respectively. The mean scores of the population for anxiety, depression and psychosomatic distress were 16.15 (SD = 5.16), 13.16 (SD = 7.93), and 6.92 (SD = 5.18). The HSCL-25 cut-off scores were 1.75 for each item of anxiety and depression.41 After applying the cut-off criteria of 17.50 for anxiety and 26.25 for depression, it was found that the prevalence of anxiety and depression among medical doctors were 30.89 % and 25.41 % respectively (see details in Table 7). 19.56% had scores above the cut-offs for both anxiety and depression 5.7% of participants obtained scores that are within the range of risk of suicide on this measure. Of the latter, 3.7% claimed to have suicidal thoughts ‘a lot’ and 2%, ‘extremely high’ in the last two weeks before responding. The somatic symptoms were calculated based on five severity categories: no to minimal (0-3), low (4-7), medium (8-11), high (12-15), and very high (16-32). The prevalence of psychosomatic measures among respondents was as follows: medium = 20.80%, high = 13.70% and very high = 6.80%. In a cumulative way, almost 40% of the respondents’ experienced high psychosomatic distress (Table 2).
|
|
|
|
Anxiety |
|
Depression |
Somatic |
|
|
Characteristic |
Sub-Heading |
N |
% |
M |
SD |
M |
SD |
M |
SD |
Overall |
Medical/Dental Doctors |
547 |
100 |
16.15 |
5.16 |
23.16 |
7.93 |
11.9 |
6.42 |
Gender |
Male |
415 |
75.9 |
16.01 |
5.14 |
22.64 |
7.62 |
11.92 |
6.35 |
Female |
129 |
23.6 |
16.68 |
5.2 |
24.95 |
8.69 |
11.91 |
6.73 |
|
Unknown |
3 |
0.5 |
12.67 |
2.31 |
18.33 |
2.89 |
9.67 |
1.15 |
|
Position |
General Physician/ Dental Doctor |
291 |
53.2 |
16.59 |
5.18 |
23.8 |
8.04 |
11.37 |
6.8 |
Consultant |
153 |
28 |
15.27 |
4.88 |
22.16 |
7.72 |
12.03 |
6.26 |
|
Senior Consultant |
39 |
7.1 |
14.49 |
5.17 |
20.69 |
7.92 |
11.64 |
4.79 |
|
Director |
9 |
1.6 |
16.56 |
5.43 |
24.22 |
6.83 |
13.78 |
6.08 |
|
Resident Doctor |
55 |
10.1 |
17.4 |
5.3 |
24.13 |
7.67 |
14.29 |
5.35 |
|
Qualification |
MBBS |
288 |
52.7 |
16.79 |
5.22 |
23.88 |
8.04 |
11.9 |
6.6 |
Master’s in Medicine |
199 |
36.3 |
15.73 |
5.27 |
22.75 |
7.92 |
12.95 |
6.12 |
|
Doctorate in Medicine |
60 |
11 |
14.5 |
3.93 |
21.1 |
7.06 |
8.47 |
5.33 |
|
Experience |
0-2 Years |
188 |
34.4 |
16.13 |
4.97 |
23.36 |
7.84 |
12.54 |
7.09 |
2-5 Years |
183 |
33.46 |
16.65 |
5.37 |
23.55 |
8.22 |
11.23 |
5.75 |
|
5-10 Years |
109 |
19.93 |
16.32 |
5.14 |
22.88 |
7.68 |
11.62 |
7.08 |
|
10+ Years |
67 |
11.88 |
14.57 |
4.92 |
22.01 |
7.84 |
12.4 |
4.78 |
|
Type of Institution |
Government Hospital |
242 |
44.24 |
16.02 |
4.99 |
23.09 |
7.47 |
11.71 |
6.03 |
Private Hospital |
175 |
31.99 |
16.1 |
5.48 |
22.88 |
8.35 |
10.29 |
6.96 |
|
Teaching Hospital |
97 |
17.73 |
16.54 |
5.04 |
23.66 |
7.8 |
14.44 |
5.58 |
|
Private Practice |
20 |
3.66 |
15.45 |
4.05 |
22.05 |
6.59 |
13.95 |
4.94 |
|
NGO/Public |
13 |
2.38 |
17.38 |
6.54 |
26.23 |
12.58 |
15.31 |
6.92 |
|
Location of Job |
Home-Based |
303 |
55.39 |
16.5 |
5.5 |
23.48 |
8.3 |
11.95 |
6.35 |
Out of Home |
244 |
44.61 |
15.72 |
4.68 |
22.77 |
7.44 |
11.85 |
6.52 |
|
Rural/Urban/ |
Out of Kathmandu Valley |
224 |
40.95 |
17.03 |
5.44 |
24.06 |
8 |
13.71 |
6.02 |
Aboard |
Kathmandu Valley |
289 |
52.83 |
15.48 |
4.86 |
22.52 |
7.93 |
10.56 |
6.48 |
Working Abroad |
34 |
6.22 |
16.06 |
5.04 |
22.65 |
7.12 |
11.44 |
5.78 |
|
Age Group |
18-25 Years |
67 |
12.25 |
18.69 |
5.82 |
26.64 |
9.55 |
12.87 |
7.88 |
26-45 Years |
451 |
82.45 |
15.93 |
5.02 |
22.86 |
7.67 |
11.82 |
6.21 |
|
46-60 Years |
26 |
4.75 |
13.81 |
3.68 |
19.96 |
5.14 |
11.31 |
5.97 |
|
60+ Years |
3 |
0.55 |
13.67 |
3.51 |
19 |
4 |
8.67 |
7.02 |
|
Type of Service |
Emergency Service |
97 |
17.73 |
17.61 |
5.73 |
24.48 |
8.27 |
13.31 |
6.6 |
Out-Patient |
36 |
6.58 |
14.83 |
4.11 |
20.47 |
5.15 |
5.25 |
4.56 |
|
Surgery/Post-Op. |
225 |
41.13 |
15.65 |
5.06 |
22.81 |
8.04 |
12.74 |
5.78 |
|
Private Clinic |
89 |
16.27 |
15.66 |
4.9 |
22.46 |
7.8 |
8.7 |
6.5 |
|
Other |
74 |
13.53 |
16.82 |
5.33 |
24.7 |
8.7 |
13.74 |
5.87 |
|
All of the Above |
26 |
4.8 |
16.65 |
4.44 |
23 |
5.69 |
14.42 |
5.01 |
|
Caseload per Week |
Below 25 |
124 |
22.67 |
15.1 |
4.58 |
22.03 |
7.65 |
8.44 |
5.98 |
26-49 |
153 |
27.97 |
16.26 |
5.01 |
22.92 |
7.77 |
10.48 |
6.89 |
|
50-75 |
120 |
21.94 |
16.38 |
5.42 |
23.3 |
7.79 |
14.68 |
5.4 |
|
76 or above |
150 |
27.42 |
16.73 |
5.47 |
24.23 |
8.35 |
14 |
5.23 |
|
Clinical Supervision |
Not Heard of |
62 |
11.33 |
16.5 |
5.05 |
24.5 |
7.88 |
15.08 |
6.41 |
Yes |
169 |
30.9 |
15.9 |
4.97 |
22.62 |
7.74 |
13.25 |
5.75 |
|
No |
316 |
57.77 |
16.22 |
5.29 |
23.19 |
8.03 |
10.56 |
6.42 |
|
Self-Care Training |
Not Heard of |
50 |
9.14 |
16.08 |
4.88 |
24.14 |
7.92 |
13.86 |
6.07 |
Yes |
30 |
5.48 |
15.27 |
5.19 |
21.33 |
6.97 |
9.37 |
6.39 |
|
|
No |
467 |
85.37 |
16.22 |
5.19 |
23.17 |
7.98 |
11.86 |
6.41 |
Table 2 Distribution of Distress Measures across Socio-Demographic Variables
There was a significant difference in depression scores according to the gender, qualifications, and age group of the respondent and the location of the services he or she provided. The one-way analysis of variances (ANOVA) showed that the depression scores for gender were significantly different from [F (2, 544) = 4.818, p = 0.008]. The post hoc Tukey test verified significant differences, with small effects, between the depression scores of males and females with (p = 0.01, d = 0.28). Depression scores also varied significantly according to the qualifications and age groups of the respondents.
One-way ANOVA results showed that, age-group-wise, group differences were [F (3,543) = 6.396, p = 0.001]. The post hoc Tukey test showed that the mean score of depression of doctors group with the age of 18-25 years, 26-45 years, and 46-60 years differed significantly (p = 0.001), but the depression score of the age group (60 + years) did not show any significant difference with other age groups. The differences on the depression scores between 18-25 years and 26-45 years of age group was significant with a medium effect (p = 0.001, d = 0.44), however, the differences on the depression scores between 18-25 years and 46-60 years of age groups were significant with very large effect (p = 0.001, d = 0.87). Similarly, the variation on the mean score of depression between 26-45 years and 46-60 years of age groups of doctors were significant with (p = 0.001, d = 0.44). Qualification-wise, one-way ANOVA showed that the differences on depression scores were [F (2, 544) = 3.49, p = 0.031]. Post hoc Tukey test outlined a significant difference in the depression scores between MBBS and Doctor of Medicine groups with a median effect (p = 0.036, d = 0.37), but the rest of the qualification wise group had no significant differences in their depression mean scores.
Applying one-way ANOVA revealed that the prevalence of anxiety was significantly different in terms of qualification, age group, and location of service: [F (2,544) = 6.045, p = 0.003], [F (3,543) = 7.993, p < 0.001], [F =2,544) = 5.800, p = 0.003]. The post hoc Tukey test for qualification outlined, the anxiety scores of MBBS and Doctor of Medicine groups were significantly different with a median effect (p = 0.005, d = 0.50), but the rest of the qualification wise group had no significant differences in their anxiety mean scores. Similarly, a post hoc Tukey test analyzed the anxiety scores of age groups and found, a significant and high effect difference on the anxiety scores of 18-25 years group with 26-45 years (p <0.001, d = 0.51). Whereas, the difference between 46-60 years of age group was significant with a medium effect (p < 0.001, d = 0.48). There were no significant differences in the anxiety mean scores of other age groups. A post hoc Tukey test for location of service and anxiety scores were tested, the anxiety scores of doctors working outside of Kathmandu Valley were significantly different, with a median effect, with the doctors working inside the Kathmandu valley (p = 0.003, d = 0.37).
The participants’ scores for somatic symptoms were significantly different across position, qualification, type of institution, type of service provided, weekly caseload, availability of clinical supervision, and self-care training. The one-way ANOVA results for position, qualification, and type of institution were [F (4,542) = 2.660, p = 0.032], [F (2, 544) = 11.698, p < 0.001] and [F (4,542) = 8.487, p = 0.003] respectively. Position wise a post hoc Tukey test was conducted, in which, the mean score of the psychosomatic burden of general physician and resident were only found significantly different with a medium effect (p = 0.017, d = 0.48). The rest of the groups were found with no significant differences in psychosomatic scores. Qualification wise, the psychosomatic scores of MBBS with Doctor of Medicine group were significantly different with a median effect (p <0.001, d = 0.57), and the group of doctors with a master’s Degree in Medicine were significantly different with a median effect ((p <0.001, d = 0.78), with the group of Doctor of Medicine. There was no significant difference in the psychosomatic mean scores between MBBS and master’s Degree in Medicine groups.
A post hoc Tukey test results for Type of Institutions group-wise differences on psychosomatic burden was tested. The mean score of psychosomatic burden between the doctors working in the teaching hospital was significantly different with a median effect than doctors working in government hospitals (p = 003, d = 0.47). Similarly, the group of doctors working in teaching hospitals had higher psychosomatic mean scores with significant and medium effect on the psychosomatic burden than the doctors working in private hospitals (p <0.001, d = 0.65). The psychosomatic burden of the doctors working in the NGO/public sector was significantly higher, with a median effect than the doctors working in private hospitals (p = 0.043, d = 0.72). The mean scores on the psychosomatic burden with other groups were found non-significant.
The significant differences with among somatic symptom scores for type of service, weekly caseload, clinical supervision, and self-care training were [F (5,541) = 18.397, p < 0.001], [F (3, 543) = 31.987, p < 0.001], [F (2, 544) = 19.472, p < 0.001], and [F (2, 544) = 4.736, p = 0.009] respectively.
A post hoc Tukey test for type of service group was carried out. The doctors working in emergency service had significantly higher psychosomatic burden as compared to the doctors working in Out-Patient (p < 0.001, d = 1.42), and private practice (p <0.001, d = 0.70). Similarly, the doctors working in Surgery or Post-Operative cases reported significantly higher psychosomatic burden with a large effect as compared to the doctors working in Out-Patient (p < 0.001, d = 1.44), and a moderate effect with the doctors from private practice (p < 0.001, d = 0.66). Other groups of the doctors had also significantly higher with a larger effect on psychosomatic burden as compared to the doctors working in outpatient wards ((p < 0.001, d = 1.91) and practice (p < 0.001, d = 0.98).
Post hoc Tukey test for the psychosomatic burden of doctors with various numbers of clients per week was tested. The mean psychosomatic scores of doctors serving more than 75 clients per week were statistically significant with higher scores than their counterparts: below 25 clients per week (p <0.001, d = 0.99), 26-50 clients (p <0.001, d = 0.56), whereas, there were no significant differences with the group of doctors serving 50-75 clients per week. Nevertheless, doctors serving 50-75 clients per week had significantly higher psychosomatic mean scores than the doctors serving below 25 clients per week (p <0.001, d = 1.08) and 26-50 clients (p <0.001, d = 0.67). Similarly, a significant difference on psychosomatic mean score was measured between the groups serving below 25 clients per week and 26-50 clients (p <0.001, d = 0.32).
The availability of clinical supervision should have a direct impact on the psychosomatic burden as compared to those without having such facilities. Interestingly, a reverse outcome was measured. A post hoc Tukey test outlined that doctors without clinical supervision expressed statistically significant and higher mean scores on psychosomatic than the doctors with clinical supervision (p <0.001, d = 0.44). The group with no clinical supervision and never heard about clinical supervision had significantly different with a moderate effect of differences in the psychosomatic burden (p <0.001, d = 0.30). There were no significant differences in the mean scores of the psychosomatic between the group with the availability of clinical supervision and never heard about the clinical supervision. However, the post hoc Tukey test confirmed that doctors received a self-care training had significantly lower mean scores for psychosomatic than the group of doctors who never heard of a self-care training (p = 0.007, d = 0.70). Nevertheless, there was no significant difference measured between the group of doctors having self-care training or not.
In summary, the prevalence and impact of depression were higher on female doctors, doctors below the age of 25 and undergraduate doctors than on other groups, and doctors below 25 years of age, undergraduate doctors and doctors working outside of Kathmandu valley were highly affected with anxiety. The psychosomatic burden was highest on resident doctors, directors, post-graduate medical doctors, and doctors working in teaching and private hospitals. Doctors working in surgery or post-operative departments, working with diverse categories of clients, and delivering support to over 50 clients per week had a greater somatic burden than their fellow doctors. Doctors without clinical supervision or self-care training also faced higher psychosomatic burdens than others.
Prevalence of professional quality of life measures in nepali medical doctors
The reliability coefficients of the subscales of Nepali version of ProQOL-5(BO, STS, and CS) were 0.693, 0.766, and 0.861 respectively. The overall means and standard deviations were BO (M = 31.52, SD = 4.55), STS (M = 27.92, SD = 6.50) and CS (M = 54.03, SD = 8.38). The ProQOL manual (Stamm, 2010) recommends using these cut-off criteria: for BO and STS, an overall score of 22 or less represents low risk, while an overall score of 42 or above is high risk. Scores from 22 to 42 are classified as medium risk for both BO and STS (Table 3).
Sub-Scale |
Group |
|
N |
|
% |
Interpretation Criteria |
|
BO |
Low Risk |
19 |
3.47 |
Overall score 22 or less |
|||
Medium Risk |
521 |
95.25 |
Overall score 22 to 42 |
||||
High Risk |
7 |
1.28 |
Overall score 42 or more |
||||
Overall |
547 |
100 |
Medium Risk (M = 31.52, SD = 4.55) |
||||
STS |
Low Risk |
121 |
22.12 |
Overall score 22 or less |
|||
Medium Risk |
417 |
76.23 |
Overall score 22 to 42 |
||||
High Risk |
9 |
1.65 |
Overall score 42 or more |
||||
Overall |
547 |
100 |
Medium Risk (M = 27.92, SD = 6.50) |
||||
CS |
Low Satisfaction |
1 |
0.18 |
Overall score 22 or less |
|||
Medium Satisfaction |
35 |
6.4 |
Overall score 22 to 42 |
||||
High Satisfaction |
511 |
93.42 |
Overall score 42 or more |
||||
Overall |
|
547 |
|
100 |
|
High Satisfaction (M = 54.03, SD = 8.38) |
|
Table 3 Prevalence of Professional Quality of Life Factors of Nepali Doctors (N = 547)
The mean scores of BO and STS indicate that the majority of Nepali doctors suffer from a moderate risk of both BO and STS with BO (M = 31.52, SD = 4.55) and STS (M = 27.92, SD = 6.50). Similarly, an overall score of 22 or less on the CS measure is classified as a low level of satisfaction and an overall score of 42 or above is considered as highly satisfied.
The study found that Nepali doctors are highly satisfied by providing compassionate care to their patients and caregivers: CS (M = 54.03, SD = 8.38). However, 1.28% of doctors are at high risk of BO and 1.65% face a high risk of STS. Only 0.18% doctor said that they were dissatisfied in the provision of compassionate care through the professional service (see Table 4 for details).
|
|
|
|
BO |
|
STS |
|
CS |
|
Characteristic |
Sub-Heading |
N |
% |
M |
SD |
M |
SD |
M |
SD |
Overall |
Medical/Dental Doctors |
547 |
100 |
31.52 |
4.55 |
27.92 |
6.5 |
54 |
8.38 |
Gender |
Male |
415 |
75.9 |
31.62 |
4.74 |
27.77 |
6.57 |
54.1 |
8.28 |
Female |
129 |
23.6 |
31.29 |
3.9 |
28.46 |
6.27 |
54.1 |
8.72 |
|
Unknown |
3 |
0.5 |
27.33 |
3.05 |
25.67 |
6.11 |
48.7 |
8.33 |
|
Position |
MBBS |
291 |
53.2 |
31.46 |
4.3 |
29.01 |
6.33 |
53.2 |
8.37 |
Consultant |
153 |
28 |
32.01 |
4.78 |
27.52 |
6.53 |
54.4 |
8.8 |
|
Senior Consultant |
39 |
7.1 |
29.72 |
4.39 |
23.77 |
6.39 |
54.7 |
6.92 |
|
Director |
9 |
1.6 |
30.78 |
3.6 |
26.56 |
4.75 |
56.9 |
4.31 |
|
Resident Doctor |
55 |
10.1 |
31.91 |
5.2 |
26.45 |
6.12 |
56.5 |
8.23 |
|
Qualification |
MBBS/BS in Dental |
288 |
52.7 |
31.43 |
4.73 |
28.85 |
6.29 |
53.5 |
8.61 |
Master’s in Medicine |
199 |
36.3 |
31.49 |
4.54 |
26.27 |
6.53 |
55.7 |
7.9 |
|
Doctorate in Medicine |
60 |
11 |
32.05 |
3.68 |
28.93 |
6.39 |
51.3 |
7.85 |
|
Experience |
0-2 Years |
188 |
34.4 |
31.61 |
4.52 |
28.64 |
6.18 |
53.2 |
8.59 |
2-5 Years |
183 |
33.46 |
31.6 |
4.36 |
28.15 |
6.26 |
54.5 |
8.06 |
|
5-10 Years |
109 |
19.93 |
32 |
4.82 |
28.63 |
6.71 |
54 |
9.17 |
|
10+ Years |
67 |
11.88 |
30.31 |
4.64 |
24.1 |
6.49 |
55.2 |
7.15 |
|
Type of Institution |
Govt. Hospital |
242 |
44.24 |
31.14 |
4.3 |
27.48 |
6.32 |
53.6 |
8.03 |
Private Hospital |
175 |
31.99 |
31.31 |
4.31 |
29.56 |
6.14 |
52.1 |
8.68 |
|
Teaching Hospital |
97 |
17.73 |
33 |
5.23 |
26.94 |
6.95 |
57.6 |
6.8 |
|
Private Practice |
20 |
3.66 |
30.15 |
4.96 |
23.55 |
5.57 |
56 |
9.48 |
|
NGO/Public |
13 |
2.38 |
32.69 |
4.44 |
28.08 |
7.26 |
58.2 |
10.2 |
|
Location of Job |
Home Based |
303 |
55.39 |
31.55 |
4.84 |
27.8 |
6.79 |
54.4 |
8.77 |
Out of Home |
244 |
44.61 |
31.49 |
4.17 |
28.07 |
6.12 |
53.6 |
7.87 |
|
Rural/Urban/Aboard |
Out of Kathmandu |
224 |
40.95 |
31.57 |
4.84 |
26.95 |
6.33 |
55.4 |
7.83 |
Kathmandu Valley |
289 |
52.83 |
31.45 |
4.43 |
28.76 |
6.56 |
52.7 |
8.65 |
|
Working Abroad |
34 |
6.22 |
31.82 |
3.66 |
27.21 |
6.18 |
56.3 |
7.69 |
|
Age Group |
18-25 Years |
67 |
12.25 |
30.85 |
4.45 |
30.28 |
6.18 |
54 |
8.57 |
26-45 Years |
451 |
82.45 |
31.65 |
4.61 |
27.73 |
6.46 |
54 |
8.42 |
|
46-60 Years |
26 |
4.75 |
30.73 |
3.68 |
24.69 |
6.18 |
54.5 |
7.8 |
|
60+ Years |
3 |
0.55 |
35 |
2 |
31.67 |
6.51 |
52.3 |
6.81 |
|
Type of Service |
Emergency Service |
97 |
17.73 |
32.57 |
4.4 |
29.25 |
6.14 |
55.5 |
7.76 |
Out-Patient |
36 |
6.58 |
30.64 |
3.74 |
31 |
4.32 |
47.6 |
5.33 |
|
Surgery or Post-Op. |
225 |
41.13 |
31.07 |
4.53 |
26.3 |
6.55 |
54.8 |
7.89 |
|
Clients at Clinic |
89 |
16.27 |
31.36 |
4.24 |
30.74 |
6.21 |
50.2 |
9.24 |
|
Other |
74 |
13.53 |
31.64 |
5.43 |
26.97 |
6.55 |
56 |
8.47 |
|
All of Above |
26 |
4.8 |
33 |
4.02 |
25.77 |
4.97 |
58.2 |
6.17 |
|
Caseload per Week |
Below 25 |
124 |
22.67 |
30.45 |
4.56 |
29.76 |
5.91 |
49.7 |
7.68 |
26-49 |
153 |
27.97 |
31.91 |
4.33 |
29.9 |
6.55 |
53 |
8.23 |
|
50-75 |
120 |
21.94 |
31.58 |
4.47 |
26.08 |
6.19 |
56.5 |
7.31 |
|
76 or above |
150 |
27.42 |
31.97 |
4.73 |
25.86 |
6.12 |
56.7 |
8.3 |
|
Clinical Supervision |
Not Heard of |
62 |
11.33 |
32.85 |
4.85 |
26.19 |
6.2 |
55.9 |
7.94 |
Yes |
169 |
30.9 |
31.25 |
4.77 |
26.33 |
6.63 |
55.7 |
8.01 |
|
No |
316 |
57.77 |
31.41 |
4.34 |
29.11 |
6.24 |
52.8 |
8.46 |
|
Self-care training |
Not Heard of |
50 |
9.14 |
33.2 |
4.97 |
26.68 |
6.12 |
56.9 |
8.56 |
Yes |
30 |
5.48 |
30.27 |
5.74 |
28.77 |
6.29 |
50.2 |
9.46 |
|
|
No |
467 |
85.37 |
31.42 |
4.39 |
28 |
6.54 |
54 |
8.19 |
Table 4 Distribution of PROQOL Measures across Socio-Demographic Variables
The variance of BO, STS, and CS by socio-demographic variables was tested using ANOVA. The mean values of BO, STS, and Cs for each subtype of socio-demographic variable are presented in Table 4. The BO scores were found significantly different depending on the type of institutions respondents worked for, the number of clients they served per week, and clinical supervision: the ANOVA results were [F (4,542) = 3.832, p = 0.004], [F (3,543) = 3.174, p = 0.024], [F (2,544) = 3.083, p = 0.047] respectively. No significant differences were measured for BO scores with other variables.
A post hoc Tukey test was applied. The doctors working in teaching hospitals were found statistically significantly higher BO mean scores as compared with their government hospital counterparts (p = 0.006, d = 0.38). Equally, doctors working in teaching hospitals have shown a significantly higher BO mean scores than the doctors working in private hospitals (p = 0.026, d = 0.35). No other groups had statistically significant differences in their BO mean scores. Post hoc Tukey test for the BO of doctors serving with various numbers of clients per week was tested. The BO mean scores of Doctors serving more than 75 clients per week were statistically significant with higher scores than their counterparts: below 25 clients per week (p = 0.04, d = 0.33), and 26-50 clients (p =0.031, d = 0.33), whereas, there were no significant differences with the group of doctors serving 50-75 clients per week. No other groups had statistically significantly different in the mean score of BO. Post hoc Tukey test on availability of clinical supervision outlined that the group without knowing any clinical supervision had significantly higher BO mean scores as compared to the group who regularly receive clinical supervision (p = 0.046, d = 0.55). However, there were no significant differences measured in the groups receiving clinical supervision regularly versus not receiving any clinical supervision.
Differences in socio-demographic variables and STS scores were also tested. The mean scores of STS were found significantly different according to the respondents’ qualifications, the number of years of experience, type of institution they serve, age group, type of services they provide, numbers of clients they service per week and availability of clinical supervision. The differences in STS mean scores for qualification were [F (2,544) = 10.508, p < 0.001], while those for experience, type of institution, age group, and were [F (3,543) = 9.413, p < 0.001], [F (4,542) = 6.099, p < 0.001], and [F (3,543) = 5.698, p = 0.001] respectively. In terms of numbers of service type and client served per week the differences were [F (3,543) = 17.861, p < 0.001], and [F (2,544) = 13.179, p < 0.001]. No significant differences were measured for STS mean scores when other variables were considered. Post hoc Tukey test on qualification wise groups were carried out. The STS scores of MBBS with a master’s Degree in Medicine group were significantly different from a median effect (p <0.001, d = 0.40). There was no significant difference in the STS mean scores of Doctorate in Medicine groups with MBBS and master’s Degree in Medicine groups.
Through a post hoc Tukey test on the years of experiences, doctors having over 10 years of experience had significantly higher STS mean scores as compared to other groups: less than 2 years group (p <0.001, d = 0.72), 2-5 years (p <0.001, d = 0.07), and 5-10 years (p <0.001, d = 0.69). There was no statistical difference in the STS scores among other groups. A post hoc Tukey test results for Type of Institutions group-wise differences on STS was tested, the mean score of STS between the doctors working in the private hospital was significantly different with a median effect than their government counterparts (p = 010, d = 0.33), doctors in teaching hospital (p = 011, d = 0.40), and doctors working in private practice (p = 001, d = 1.03). The mean scores on the STS with other groups were found non-significant. Age group wise, the post hoc Tukey test outlined that 18-25 years age group had statistically higher and significant STS mean scores in comparison with the STS scores of 26-45 years age group (p = 0.013, d = 0.40), and 46-60 years age group (p = 0.001, d = 0.90). The mean scores on the STS with other age groups were found non-significant.
As per the post hoc Tukey test, doctors working in surgery or post-operative clients had significantly different STS mean scores. The differences of mean score of doctors working in surgery or post-operative clients with emergency service group was (p = 0.002, d = -0.46), Out-patient working group (p < 0.001, d = - 0.85), and doctors working with clients at private clinic (p < 0.001, d = - 0.70) respectively. Similarly, doctors working with clients at private practice had significantly different STS mean scores than doctors working with other clients (p = 0.002, d = 0.59). No other groups were found statistically different.
Post hoc Tukey test for the STS of doctors with various numbers of clients per week was tested. The mean scores of Doctors serving less than 25 clients per week were statistically significant with higher scores than their counterparts: 50-75 clients per week (p <0.001, d = 0.60), and 76 or above clients (p <0.001, d = 0.56), whereas, there were no significant differences with the group of doctors serving 50-75 clients per week. Nevertheless, doctors serving 50-75 clients per week had significantly higher mean scores than the doctors serving below 25 clients per week (p <0.001, d = 1.08) and 26-50 clients (p <0.001, d = 0.65). Similarly, a significant difference was measured between the groups serving 26-50 clients with doctors serving 50-75 clients per week (p <0.001, d = 0.60), and 76 or above clients (p <0.001, d = 0.64). No other groups were found significantly different in terms of mean scores of STS.
The tests between the subject effects of CS mean scores with different socio-demographic variables revealed that the CS of doctors varies significantly by qualification, type of institution served, type of service provided, weekly caseload and level of clinical supervision. All the results were significantly different. The analysis of variance between the subject results were [F (2,544) = 7.784, p < 0.001] for qualifications, [F (4,542) = 8.585, p < 0.001] for type of institution, and F (5,541) = 12.403, p < 0.001] for type of service provided. Similarly, the variances with significant differences for weekly caseload and level of clinical supervision were [F (3,543) = 22.053, p < 0.001] and [F (2,544) = 8.629, p < 0.001] respectively. No significant differences were measured for CS mean scores with respect to other variables.
Post hoc Tukey test of ANOVA on CS score across the various socio-demographic groups was measured. CS mean scores of doctors with master’s Degree in Medicine group was significantly higher with small effect as compared to the MBBS group of doctors (p = 0.012, d = 0. 26), whereas a medium effect with significant differences was measured between the master’s Degree in Medicine group and Doctor in Medicine group (p = 0.001, d = 0. 55). There was no significant difference in the mean scores of CS between the MBBS group of doctors and Doctor in Medicine group. Post hoc Tukey test outlined that the doctors working with teaching hospitals had significantly higher CS, with a medium effect, as compared to their fellows working in private (p <0.001, d = 0.71) and government hospitals (p<0.001, d = 0.54). No other groups were found significantly different in the CS mean scores.
As per the post hoc Tukey test report, doctors working in other sectors were found significantly higher CS scores, with large effects, than the doctors working with out patients (p < 0.001, d = 1.85) and clients at private practice (p < 0.001, d = 1.02). The doctors working with surgery departments had significantly higher CS than the doctors working with out patients (p < 0.001, d = 1.07) and clients at private practice (p < 0.001, d = 0.54). Similarly, doctors working in emergency department had significantly higher CS than their counterparts working for out-patients (p < 0.001, d = 1.19) and private clinics (p < 0.001, d = 0.62). There were no statistically significant variations on the mean scores of CS among the groups of doctors serving various categories of clients.
Post hoc Tukey test for the CS of doctors with various numbers of clients per week was tested. The mean scores of Doctors serving more than 76 or above clients per week were statistically significant with higher scores than their counterparts: below 25 clients per week (p <0.001, d = 0.86), and 26-50 clients (p <0.001, d = 0.44), whereas, there were no significant differences with the group of doctors serving 50-75 clients per week. Nevertheless, doctors serving 50-75 clients per week had significantly higher mean CS scores than the doctors serving below 25 clients per week (p <0.001, d = 0.89) and 26-50 clients (p <0.001, d = 0.44). Similarly, the group serving below 26-50 clients had a significantly higher CS mean scores as compared to doctors working below than 25 clients per week (p = 0.004, d = 0.41).
In the post hoc Tukey test, doctors receiving clinical supervision had a significantly higher CS mean scores as compared to the doctors without receiving any clinical supervision (p = 0.001, d = 0.35). Surprisingly, the doctors never heard of clinical supervision had significantly higher CS mean scores as compared to the doctors not receiving clinical supervision (p = 0.017, d = 0.39). However, no statistically significant difference was measured between the doctors receiving clinical supervision and doctors never heard about clinical supervision.
In summary, the ANOVA and post-hoc test results on the BO, STS and CS have outlined; doctors working in teaching hospitals had a higher level of BO than other doctors, as did doctors working in emergency wards, providing care to over 50 clients per week and working with all categories of clients. The lack of self-care training was also associated with a higher than average level of BO. STS scores were higher among young doctors and doctors over the age of 60 than other doctors. Doctors working in a private hospital, looking after clients in out-patient wards and working with all categories of clients also experienced a higher level of STS, as did doctors with no clinical supervision and working with less than 50 clients per week. Doctors who completed a post-graduate degree had higher levels of CS than other doctors, as did those working in private and teaching hospitals or the emergency department, looking after over 50 clients per week and serving diverse categories of clients. Interestingly, clinical supervision and self-care training were not associated with a higher level of CS.
Structural Equation Model of Personal and Professional Distress
A SEM of personal and professional distress was created. The latent factors were ProQOL to represent professional distress and a combination of anxiety, depression and psychosomatic burden to represent personal distress. The BO measures of ProQOL could not be justified through CFA and were removed from the SEM. STS and CS were taken as exogenous variables, and anxiety, depression and psychosomatic burden were taken as endogenous variables. Each measure contains a residual error.
Using AMOS, a path analysis was drawn for multivariate analysis. The measurement model of psychosomatic burden contains three factors (pain, cardiopulmonary, fatigue) and was adjusted accordingly in the structural model. STS and CS were assumed to have an effect on personal distress (anxiety, depression and psychosomatic burden). The relationships among the measures of professional and personal distress were tested through the SEM. The SEM drawn as per the CFA outcomes of SSS-8, HSCL-25, and ProQOL-5 is presented in.
The model outlined a total of 86 endogenous variables, 36 of which were observed and 50 of which were not, as well as 44 exogenous. The outcome of the test in AMOS outlined 666 distinct sample moments and 77 estimated parameters. The degree of freedom was 589. The overall fit indices of the initial model are presented in Table 5.
Model |
CMIN/df |
NFI |
TLI |
GFI |
CFI |
RMR |
SMRs |
RMSEA |
P-Close |
HölterKriterium |
Initial Model |
3.104 |
0.809 |
0.852 |
0.849 |
0.862 |
0.096 |
0.1545 |
.062 |
.840 |
277 |
Table 5 Fit indices of Initial Model of ProQOL and Personal Distress (N = 547, p <.001)
Note: NFI = Normed-Fit Index, TLI = Tucker-Lewis Index, GFI = Goodness-of-Fit Index, CFI = Comparative-Fit Index, RMSR = Root mean square residuals, SMRs = Standardised root mean square residuals, RMSEA = Root mean square error of approximation, HölterKriterium for number of required samples with p = 0.01
The initial model had a poor fit. The fit indices values for the default model were, χ2 = 1828.274, χ2/df = 3.104, TLI = .852, GFI = .849, CFI = .862, and RMSEA = 0.062. The chi- square value and a few other indices were within the parameters of the recommended values. However, the fit indices for TLI, GFI, and CFI were lower than the recommended cut-off values.50 Therefore, the model was modified using a maximum likelihood method for diffeent indices. These modificaiton were carried out in the next phase. The results are presented in the section below on the final model.
The final structural model of personal and professional distress was a modification of the model in Figure 1. It had a total of 139 parameters, out of which 55 were fixed and 84 were unlabeled. Eight co-variances and 44 variances were measured, and 84 variables, 44 exogenous and 42 endogenous, were outlined. A total of 666 distinct sample moments with 84 distinct parameters to estimate and 582 degrees of freedom were examined.
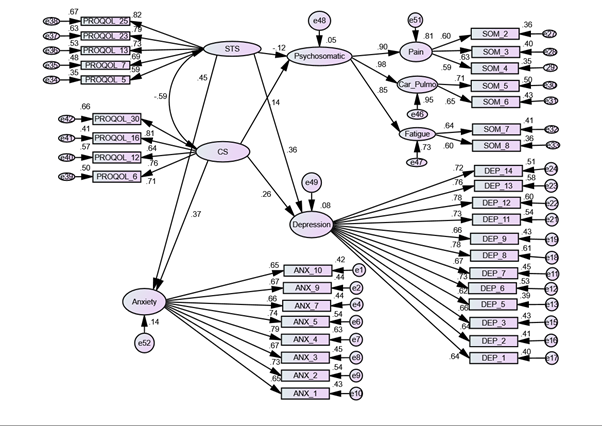
Figure 1 Initial Model of SEM for Measures of ProQOL and Personal Distress.
CS = compassion satisfaction, STS = secondary traumatic stress, DEP = depression, ANX = anxiety, SOM = psychosomatic.
The goodness-of-fit statistics for the final model (Figure 2) revealed that the error variance between and among some of the items and variables had a significant impact on the model for the best fit. Therefore, the error variances between DEP_6 and DEP_13, and DEP_7 and DEP_14 were covaried. Similarly, ANX-3 and ANX_4, ANX_4 and ANX_5, and ANX_9 and ANX_10 were covaried and adjusted. The chi-square value of the model was 1191.007, and its degree of freedom measured 582. After necessary adjustments in the modified indices, the goodness-of-fit indices in the final structural model were analysed (Table 6).
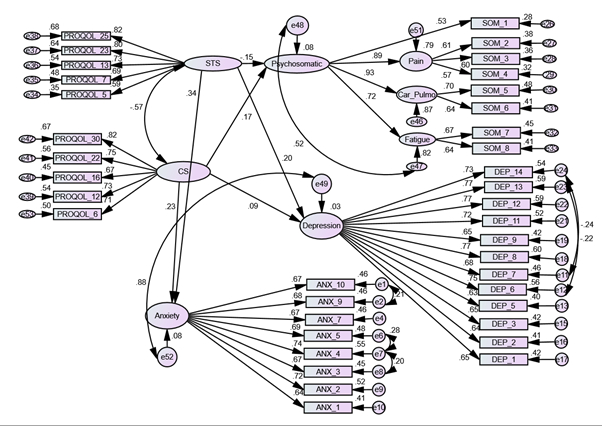
Figure 2 Final Model of SEM for Measures of ProQOL and Personal Distress.
CS = compassion satisfaction, STS = secondary traumatic stress, DEP = depression, ANX = anxiety, SOM = psychosomatic burden.
Model |
CMIN/df |
NFI |
TLI |
GFI |
CFI |
RMR |
SMRs |
RMSEA |
P-Close |
HölterKriterium |
|
2.046 |
0.876 |
0.926 |
0.888 |
0.932 |
0.052 |
0.057 |
.044 |
0.998 |
305 |
Table 6 Final ModelFit Indices for Professional and Personal Distress (N = 547, p <.001)Final ModelFit Indices for Professional and Personal Distress (N = 547, p <.001)
Note: NFI = Normed Fit Index, TLI = Tucker-Lewis-Index, GFI = Goodness-of-Fit-Index, CFI = Comparative Fit Index, RMSR = Root mean square residuals, SMRs = Standardized Root mean Square Residuals, RMSEA = Root mean square error of approximation, HölterKriterium for number of required sample with p = 0.01
The indices presented above and obtained from the analysis of the final structural model of the study have the following values: χ2 = 1191.007, χ2/df = 2.046, TLI = .926, GFI = .888, CFI = .932 and RMSEA = 0.440. Lomax and Schumacker (2004) demonstrated that chi-square values are inflated in studies with a large sample size and therefore create statistically significant chi-square results. As postulated, the test results of the final SEM show significant values of chi-square scores (p <001). The values of GFI and NFI were below the cut-off scores of .90. This model is the most optimal model for representing the professional and personal distress of Nepali doctors with the given data.
Influence of Professional Distress on Personal Distress
The influence of professional distress measures on personal distress measures was tested through path analysis. The direct effect of STS and CS on psychosomatic, depression, and anxiety are presented below. As expected, STS has a positive significant effect on depression and anxiety. The influence of STS on depression was measured at r = 0.20, R2 = 0.027, p < 0.001, while the influence of STS on anxiety was measured as r = 0.34, R2 = 0.079, p < 0.001. However, the influence of STS on psychosomatic burden was measured as negative but significant: r = - 0.15, R2 = 0.079, p = 0.028. The indirect effects on psychosomatic burden and other factors that can account for the negative effect of STS on psychosomatic burden are unknown, but the outcome did not support the theoretical concepts of correlation between STS and psychosomatic burden. The total variance (R2) for psychosomatic burden was only 8%.
Psychosomatic burden and anxiety were directly and significantly affected by CS but the impact of CS on depression, while positive, was insignificant. CS has been perceived and measured as a moderator of distress, so the significant and positive effects of CS on anxiety and psychosomatic were unexpected. The positive effect of CS on depression was also unexpected. Therefore, the hypothesis of a negative and significant effect of CS on personal distress could not be justified. The estimation of regression weights and significant estimates of various measures of personal and professional distress are presented in Table 7.
Constructs* |
Estimate |
S.E. |
C.R. |
p |
Psychosomatic <--- CS |
0.117 |
.049 |
2.394 |
0.017 |
Psychosomatic <--- STS |
-0.072 |
.033 |
-2.196 |
0.028 |
Depression <--- CS |
0.074 |
.051 |
1.445 |
0.148 |
Depression <--- STS |
0.115 |
.035 |
3.281 |
0.001 |
Anxiety <--- CS |
0.163 |
.047 |
3.501 |
<.001 |
Anxiety <--- STS |
0.164 |
.032 |
5.176 |
<.001 |
Table 7 Estimation of regression weights and significant estimates for different measures
Note: *Constructs are represented by: CS = compassion satisfaction, STS = secondary traumatic stress, psychosomatic burden, depression, and anxiety
The negative emotional state of any medical doctor has an impact on the care and services he or she provides to patients and affects his or her ProQOL.38,51 The CF and CS model of understanding the negative and positive impacts on medical doctors was chosen as the best theoretical model to assess such impacts.51 The personal distress of doctors was evaluated using the widely used measures of anxiety, depression and psychosomatic burden.42,52,53
The high level of participation, 547 doctors out of an estimated 15,000, is one strength of this study. The high rates of anxiety, depression, suicidal ideation, and psychosomatic burden found, as are presented in the results section, are corroborated by similar studies in China, Pakistan, and India.20,54,55 One out of four Nepali doctors faces the comorbidity of anxiety and depression. Suicidal ideation is high in one out of twenty doctors and one in three doctors has a high level of depression. Young doctors, female doctors, and doctors working outside of Kathmandu Valley are at risk of a high level of depression and suicide. The literature reviewed in this study also demonstrated the high rate of depression and suicide among female doctors. Suvedi et al.56 outlined, the depression and suicide burden among childbearing-aged women in Nepal is extremely high, 6% of the below 30 years. The fact that Nepali female doctors have even higher rates of depression, suggest that they undergo a great deal of social and familial distress. The prevalence of depression in the Nepali population ranges from 30.9% to 40.6%.57-60 Despite the fact that some studies in the literature review conclude that the depression and anxiety of doctors is higher than that of the general population,61 however this study findings shown, the prevalence of depression and anxiety of Nepali doctors are slightly lower than the range experienced by the general Nepali population.
The proportions of Nepali doctors at high risk of BO and STS found by this study were lower than those found in other populations of doctors in other, similar studies in developing countries.62-64 The CS of Nepali doctors is slightly higher than that found in other studies,65,66 a fact suggesting that Nepali doctors are more resilient than doctors elsewhere. However, over 50% of Nepali doctors are found at moderate risk of BO and STS. Doctors working with over 50 clients per week or without clinical supervision and young doctors working in private and teaching hospitals were found to be at risk of CF. Over 90% of Nepali doctors were found to have a high level of CS, a finding suggesting that the profession of medical doctor is a dignified one that provides satisfaction to those who provide support to patients. These findings have clearly outline huge differences on the lower job satisfaction and higher level of burnout in other studies conducted in developed countries.67,68
It is possible that family, peer and community support in developing countries like Nepal is stronger, even in clinical settings, than it is in developed countries.69-71 Only 18 doctors out of 1,000 were found to be dissatisfied with their service and profession. However, the outcomes show that Nepali doctors are at risk of CF and that preventive measures need to be put in place. As was found elsewhere, the prevalence of both professional and personal distress was higher among medical doctors with no clinical supervision, female doctors, young doctors working in private and teaching hospitals, doctors dealing with very high numbers of clients each week, and doctors who have not participated in self-care training.66,72
The influence of ProQOL measures (STS and CS) on distress (anxiety, depression and psychosomatic) measures was tested through using a SEM technique. The items for all measures except BO that were retained during the CFA process were kept as variables to fit the model. Model indices were tested. The prescribed model fit outcomes suggested a strong positive correlation between depression and anxiety scales (alpha = 0.87), a finding which supports previous findings.22 The findings suggested that the symptomatic coverage of both depression and anxiety measures were similar to the coverage of STS. STS had a linear correlation with depression and anxiety. The correlation of STS was moderately, but significantly, correlated with depression (r = 0.20, p < 0.001) and anxiety (r = 0.34, p < 0.001). Despite the theoretical understanding of positive correlations between psychosomatic and STS measures, the results showed that psychosomatic measures were poorly and negatively correlated with STS (r = - 0.15, p = 0.028). These outcomes need critical qualitative and quantitative evaluations in the future.
Surprisingly, anxiety, depression and psychosomatic measures were positively correlated with CS (Figure 3). These results, which are explored above, are the opposite of the general theoretical understanding51,38 and therefore need monitoring in future research.37,73 Studies on the professional and personal distress of Nepali doctors are very rare, so this study has many limitations to concretely explain such opposite findings. Any theoretical, cultural or social factors interlinking to such findings needs further studies. The few studies on the conceptual similarities between BO and depression symptoms in medical doctors in other contexts.74 could not be tested due to the omission of BO from the CFA due to poor model fit.
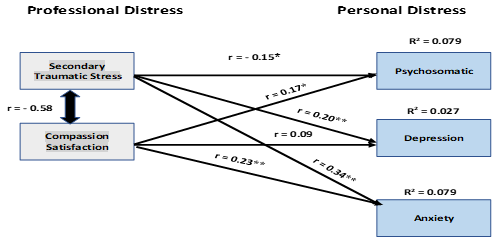
Figure 3 Path Diagram of the Influence of Professional Distress on Personal Distress.
r = effect or correlation coefficient, R2 = variance, * = p <.05, ** = p <.001.
The findings of this study in terms of measuring the impact of professional distress on personal distress have to be referenced with various limitations, and the replicability of a similar theoretical basis in another context is very low. As the interrelationships among the professional and personal distress of Nepali medical doctors were not strong, a null hypothesis on the strong influence of professional distress on personal distress could not be justified. The research findings, therefore, suggest screening both professional and personal measures at once to understand the reverse causation until other studies in future suggests differently, while providing medical care to Nepali doctors who are experiencing personal or professional distress. This study found that one out of four medical doctors in Nepal faces the challenges of anxiety and depression, a finding which indicates that it is urgent to find appropriate measures for addressing the psychological distress of medical doctors. The burden of suicide is alarming, with 2% of doctors reporting an ‘extremely high’ desire to self-harm and female doctors more affected than their male counterparts. The burdens of BO and STS are relatively low but concerns about professional distress still need proper attention.
This study has several limitations. The response rate of online respondents was difficult to trace and the response rate for the paper-and-pencil form of data collection was just under 60%. The sample size was diverse: it represented rural and urban doctors, senior and junior doctors, doctors of different ages, and doctors working at different types of institutions. The targeted sample size was fulfilled, but doctors in remote areas without internet facility may have been left out.75 The data collection tools, mainly ProQOL-5, were translated into Nepali and tested on mental health and psychosocial support professionals. The use of non-validated tools, both SSS-8 and ProQOL-5, pose certain limitations on the replicability of the findings. In any online survey, the respondent generally provides a socially desirable answer, a tendency which is often difficult to control but which impacts study outcomes.76 A cross-sectional survey design has many limitations. Such a study cannot provide insight into the causation of a problem.77,78 Because the data was cross-sectional, a diverse range of socio-demographic variables such as age, gender, type of institution, and level of support (supervision, training, etc.) was compared to present the significant differences in the outcomes of both personal and professional distress. Nevertheless, it was difficult to measure the causation of such differences. In terms of the ethical ground of the research, using a cross-sectional design prevented participants’ form being repeated exposed to distress measures, as is generally the case with a longitudinal design.
Ultimately, the findings of this research do not provide a causal link with respect to the significant differences in the outcomes of both personal and professional distress. The studied population is highly educated and represents the higher strata of socio-economic groups in Nepali society. The researcher clearly outlined in the inclusion criteria that the respondent should be fluent in English and Nepali language. Since most of the doctors had probably studied in English language medium institutions since high school, some of the terminology translated into Nepali on the data collection tools may have been difficult for them to fully understand. Thus, the results based on the collected data and its analysis might have some bias in this regard. The study findings must be analysed with such caveats in mind.
The study concludes a reiteration of the high prevalence of personal distress, moderate risk of CF, and high compassion satisfaction among Nepali medical doctors. A strong influence of professional distress measures on personal distress measures was not verified. The study concludes that further research on the influence of and interrelationships among measures of professional and personal distress in the population of medical doctors is needed. It also suggests screening both personal and professional distress while providing treatment and care to medical doctors. Despite having some methodological, statistical, and practical limitations, this study provides ample opportunities for understanding the professional and personal distress among Nepali doctors, the interrelationships among the measures of distress, and the applicability of the adapted tools. The study outcomes also suggest that screening for personal distress (anxiety, depression and psychosomatic burden) is important while looking at the professional distress of medical doctors in clinical settings. The study findings also show that there is an immediate need for action in addressing the distress of doctors to sustain the limited workforce and provide uninterrupted good-quality care to patients and exploring the qualitative aspects of distress faced by the Nepali doctors.79-96
This research was carried out as a component of the researcher’s Ph.D. degree in Psychology at the University of Nicosia. Thanks Dr. Martin Nechtelberger’s encouragement and guidance at every step. I am grateful for the support and encouragement of Dr. Nuno Ferreira, Coordinator of the Ph.D. programme at the Psychology Department. Gratitude to all the medical doctors who participated in and contributed to this study. Two institutions, Rhythm Neuro-Psychiatry Hospital and Research Center and Transcultural Psychosocial Organisation (TPO Nepal), are thankful for their institutionalised support in providing mental health and psychological support to respondents in need. Deepest gratitude goes to senior Nepali psychologist Mr. Bhava Poudyal, psychologist Mr. Sujen Man Maharjan, and Nepali language expert Hemraj Adhikari for their invaluable support for the process of culturally adapting the research tools. I am thankful to two social workers, Mr. Raaz Chhetri and Ms. Sumina Machamasi, for their support in collecting paper-and-pencil responses from respondents.
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
None.

©2022 Adhikari, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.
 World Eating Disorder Week is observed from 23 February 2026 to 01 March 2026 to increase awareness of eating disorders and their psychological impact, and to promote early intervention and recovery. This initiative highlights the role of psychology and clinical psychiatry in understanding and treating eating disorders.
Researchers are encouraged to submit relevant research articles, reviews, and clinical findings. Submissions received during this week will receive a 30–40% publication discount in the Journal of Psychology & Clinical Psychiatry (JPCPY).
.
World Eating Disorder Week is observed from 23 February 2026 to 01 March 2026 to increase awareness of eating disorders and their psychological impact, and to promote early intervention and recovery. This initiative highlights the role of psychology and clinical psychiatry in understanding and treating eating disorders.
Researchers are encouraged to submit relevant research articles, reviews, and clinical findings. Submissions received during this week will receive a 30–40% publication discount in the Journal of Psychology & Clinical Psychiatry (JPCPY).
.