MOJ
eISSN: 2374-6939


Technical Paper Volume 17 Issue 5
1Grupo de Oncologia Ortopédica do Serviço de Ortopedia e Traumatologia da Santa Casa de Porto Alegre, Brasil
2Irmandade Santa Casa de Misericórdia de Porto Alegre (ISCMPA), Brasil
3Universidade Federal de Ciências da Saúde de Porto Alegre (UFCSPA), Brasil
Correspondence: Igor Casotti de Pádua, Universidade Federal de Ciências da Saúde de Porto Alegre Rua Tomaz Flores, 82 –Apto 503 – CEP 90035-200, Porto Alegre, Rio Grande do Sul, Brasil, Tel +55 (44)997434378
Received: October 23, 2025 | Published: November 11, 2025
Citation: David A, Alimena LJM, Birriel FC, et al. Contribution to the technique of proximal limb disarticulations and amputations: suspended positioning and asynchronous vascular ligation. MOJ Orthop Rheumatol. 2025;17(5):147-149. DOI: 10.15406/mojor.2025.17.00724
Background / Objective: Proximal disarticulations and amputations remain necessary for selected cases of locally advanced extremity tumors. We describe a modified technique combining suspended limb positioning, simultaneous two-team dissection, and asynchronous vascular ligation, and report outcomes from an initial case series.
Methods: Retrospective case series at a single orthopedic oncology referral center including all consecutive patients who underwent the described procedure between 1999 and 2020. Demographic, histologic and perioperative data were collected. The study was approved by the institutional ethics committee (Opinion No. 7.316.148).
Results: Eighteen patients were included (11 males, 7 females; mean age 54.4 years, range 13–92). Most common diagnoses were chondrosarcoma (n=7), pleomorphic sarcoma (n=4) and osteosarcoma (n=3). All patients survived at least 30 days postoperatively. The technique was feasible and safe in this series; the combined strategy appeared to improve surgical exposure and hemostatic control, in line with existing reports.
Conclusions: Suspended limb positioning with a simultaneous two-team approach and asynchronous vascular ligation is a safe, reproducible, and ergonomically advantageous method for proximal amputations in orthopedic oncology, with potential to optimize operative time and blood loss. Prospective comparative studies are warranted to validate these findings.
Keywords: hip disarticulation, proximal amputation, limb suspension, asynchronous vascular ligation, orthopedic oncology, surgical technique
With advancements in neoadjuvant chemotherapy and reconstruction techniques, limb-sparing surgery has become the gold standard for treating most extremity sarcomas. Nevertheless, proximal amputations, such as hip disarticulation, hemipelvectomy, and interscapulothoracic amputation, remain essential last-resort procedures for cases of locally advanced tumors with extensive neurovascular involvement, refractory infection, or failure of a previous limb-sparing surgery.1
Such procedures are associated with substantial perioperative morbidity, including significant blood loss, long surgical times, and high complication rates, which can reach up to 44%. Conventional approaches, such as that described by Sugarbaker for hip disarticulation, often require one or two assistants dedicated exclusively to limb manipulation, which can be ergonomically challenging and hinder surgical access.2 Furthermore, patient positioning can lead to venous congestion, exacerbating blood loss.
To mitigate these challenges, we have developed a modified technical approach based on three fundamental principles: (1) optimization of surgical field exposure through suspended limb positioning; (2) enhancement of surgical efficiency by the simultaneous action of two experienced surgeons; and (3) minimization of blood loss through asynchronous vascular ligation. This last principle, which consists of early arterial ligation followed by delayed venous ligation to allow for passive drainage of the limb, has been shown to significantly reduce blood loss and operative time in hip disarticulations.3 The objective of this study is to describe this combined technique in detail and to report the clinical and surgical outcomes of an initial series of 18 patients treated at our institution.
Study design and ethical approval
A retrospective case series study was conducted at a single reference center for orthopedic oncology. The study was approved by the institution's Research Ethics Committee (Opinion No. 7.316.148; CAAE: 83678824.2.0000.5335), with a waiver of the Informed Consent Form, given the retrospective nature of the medical record analysis.
Patient cohort
All consecutive patients diagnosed with primary or secondary malignant neoplasms in the upper or lower limbs who underwent disarticulation or proximal amputation using the described technique between 1999 and 2020 were included. The demographic and clinical characteristics of the 18 included patients are detailed in Table 1.
|
Patient |
Age (years) |
Sex |
Histopathological diagnosis |
Surgical procedure (Example) |
|
1 |
49 |
Female |
Liposarcoma |
Hip Disarticulation |
|
2 |
79 |
Female |
Pleomorphic Sarcoma |
Hip Disarticulation |
|
3 |
35 |
Male |
Squamous Cell Carcinoma |
Interscapulothoracic Amputation |
|
4 |
13 |
Male |
Osteosarcoma |
Hip Disarticulation |
|
5 |
76 |
Male |
Synovial Sarcoma |
Hip Disarticulation |
|
6 |
21 |
Male |
Chondrosarcoma |
Hip Disarticulation |
|
7 |
54 |
Female |
Chondrosarcoma |
Hip Disarticulation |
|
8 |
18 |
Male |
Osteosarcoma |
Hip Disarticulation |
|
9 |
43 |
Male |
Pleomorphic Sarcoma |
Hip Disarticulation |
|
10 |
62 |
Male |
Chondrosarcoma |
Hip Disarticulation |
|
11 |
43 |
Male |
Pleomorphic Sarcoma |
Hip Disarticulation |
|
12 |
64 |
Male |
Chondrosarcoma |
Hip Disarticulation |
|
13 |
66 |
Female |
Pleomorphic Sarcoma |
Hip Disarticulation |
|
14 |
71 |
Female |
Osteosarcoma |
Proximal Transfemoral Amputation |
|
15 |
28 |
Male |
Chondrosarcoma |
Hip Disarticulation |
|
16 |
69 |
Female |
Chondrosarcoma |
Hip Disarticulation |
|
17 |
87 |
Male |
Plasmacytoma |
Proximal Transfemoral Amputation |
|
18 |
92 |
Female |
Chondrosarcoma |
Hip Disarticulation |
Table 1 Demographic and Clinical Characteristics of Patients (n=18).
Surgical technique
The procedure requires the presence of two senior surgeons familiar with the regional anatomy.
Anesthesia and preparation: After the induction of general anesthesia, central venous access is obtained and a Foley catheter is placed. The patient is then positioned in lateral decubitus, with the affected limb facing upward. The surgical table is adjusted to an ergonomic height for both teams.
Limb positioning and suspension: The distal extremity of the limb (foot or hand) is wrapped with a crepe bandage, which is then attached to a sturdy hook secured to the operating room ceiling. The limb is elevated to achieve approximately 30 to 45 degrees of abduction relative to the trunk (Figure 1-4). This positioning is analogous to that used in complex shoulder girdle procedures and aims to create a static surgical field with 360° circumferential access to the root of the limb, in addition to promoting passive venous drainage.4,5
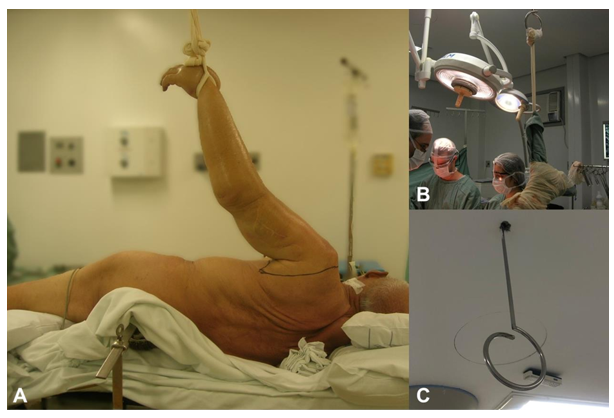
Figure 1 Patient positioned with the limb abducted 45 degrees, the wrist tied to a ceiling hook (A). Hook and tie with the limb already removed (B). Detail of the hook fixed to the operating room ceiling (C).

Figure 2 Disarticulated limb, after removal, on a separate sterile table while the team performs closure of the surgical wound.
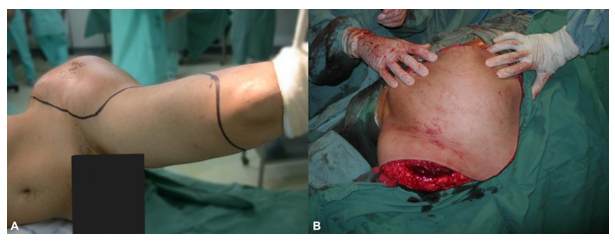
Figure 3 Lower limb suspended at leg level, with the incision to be made (A). Detail of the flap over the operative wound (B).
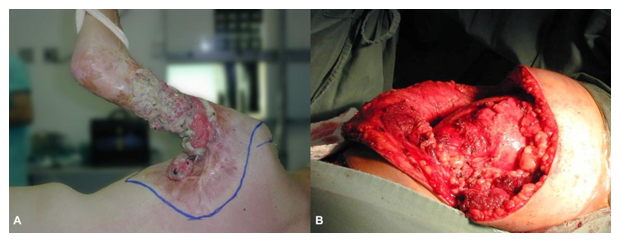
Figure 4 Patient with squamous cell carcinoma at the root of the left upper limb (LUL), in lateral decubitus and tied to the ceiling (A). Operative wound after limb removal (B).
Antisepsis and surgical approach: Antisepsis is performed in the usual manner, and surgical drapes are positioned to isolate the suspension tie. The primary surgeon is positioned on the side containing the main neurovascular bundle (usually ventral/anterior), while the second surgeon is positioned on the opposite side (dorsal/posterior). The skin incision is marked according to the oncologic plan to ensure adequate margins. Both teams begin dissection simultaneously, each with their own assistant, electrocautery, and suction system.
Vascular management (Asynchronous ligation): The primary surgeon's first objective is the identification and early ligation of the main artery of the limb. After the interruption of arterial flow, the dissection of muscular and neural planes proceeds. This maneuver allows for passive venous blood drainage from the limb, optimized by gravitational elevation. The main vein is approached and ligated only in a later phase of the procedure, at which point it appears visibly collapsed. This strategy has been proven effective in reducing intraoperative blood loss.3
Resection and closure: After the transection of all structures, the disarticulation or osteotomy is completed, and the surgical specimen is removed. The closure of the surgical wound follows standard principles, with rigorous hemostasis, insertion of suction drains, and layered suture.
The case series consisted of 18 patients, 11 (61.1%) male and 7 (38.9%) female, with a mean age of 54.4 years (range: 13 to 92 years). The most common histopathological diagnosis was chondrosarcoma (n=7; 38.9%), followed by pleomorphic sarcoma (n=4; 22.2%) and osteosarcoma (n=3; 16.7%). Individual demographic and clinical details are summarized in Table 1. Postoperative follow-up of the patients confirmed a perioperative survival of at least 30 days for all individuals in the series.
This study describes a combined technical approach for proximal amputations in orthopedic oncology, which proved to be safe and feasible in a series of 18 cases.6–9 The main innovation lies in the synergy of three components: suspended limb positioning, a simultaneous two-team approach, and asynchronous vascular ligation. Preliminary results suggest that this approach may optimize surgical efficiency and hemostatic control. The primary ergonomic advantage of limb suspension is the creation of a static surgical field with 360° circumferential access, eliminating the need for an assistant for manipulation and allowing for an unimpeded, simultaneous approach by two surgical teams.10 This not only reduces personnel demand but may also decrease team fatigue and potentially shorten surgical time. This positioning, analogous to that used in interscapulothoracic amputations, also elevates the limb above the level of the heart, promoting passive venous drainage and contributing to the reduction of blood loss, a fundamental principle in surgical bleeding control.11
The most impactful component for hemostasis is likely the asynchronous vascular ligation. By ligating the artery early and the vein late, the technique utilizes gravity and residual arterial pressure to "exsanguinate" the limb into the patient, functioning as a passive autotransfusion. The efficacy of this maneuver was validated by Wang et al. (2022), who, in a comparative study of 20 hip disarticulations, demonstrated that delayed venous ligation resulted in a significantly shorter operative time (123 vs. 154 min) and lower total blood loss (1007 vs. 1735 mL) compared to synchronous ligation. Our results appear to corroborate these findings. This study has limitations inherent to its design. As a retrospective, single-center case series, it lacks a control group for direct comparison, and the sample size is small. The heterogeneity of diagnoses and procedures performed may also influence the results. Therefore, the observed advantages regarding surgical time and blood loss, although promising, should be interpreted with caution. Prospective and, ideally, randomized studies would be necessary to confirm the superiority of this technique over conventional approaches.
The technique of suspended positioning combined with a two-team approach and asynchronous vascular ligation represents a safe, reproducible, and effective approach for disarticulations and proximal amputations in orthopedic oncology. The technique offers ergonomic advantages and appears to optimize surgical time and hemostasis. Although the results of this initial series are encouraging, future comparative studies are necessary to fully validate its benefits.
Each author contributed significantly to the development of this article: AD, LJMA, FCB: Conceptualization, Methodology, Investigation, Data Curation, Formal Analysis, Validation, Visualization, Writing - original draft, -Writing - review & editing. ICP, WP: Writing - original draft, Writing - review & editing.
The authors declare that there are no conflict of interest.

©2025 David, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.