Journal of
eISSN: 2373-6437


Case Report Volume 12 Isuue 3
1Senior House Officer, Townsville University Hospital - Anaesthetics Department 100 Angus Smith Dr, Australia
2Anaesthetics Consultant; MD, Fellow of ANZCA, Fellow of CICM, Australia
3Anaesthetics Fellow; MBBS Grad Cert Med (CritCare), Australia
Correspondence: Lachlan Young, Senior House Officer MD, 10 Chandon Place, Castle Hill, Queensland 4810, Australia, Tel +614 1008 1016
Received: May 12, 2020 | Published: May 25, 2020
Citation: Young L, 1Potgieter D, Roche C. Successful intubation of a treachercollins syndrome patient with ‘STRIVE Hi’ and videolaryngoscopy: a case report. J Anesth Crit Care Open Access. 2020;12(3):105-107. DOI: 10.15406/jaccoa.2020.12.00441
Treacher Collins Syndrome (TCS) is characterised by craniofacial abnormalities which pose a unique airway challenge for anesthetists. This case report presents a TCS patient with profound retrognathia and restricted oral opening requiring emergent bile duct exploration. Given the requirement for general anesthesia and preference of endotracheal intubation, maintaining spontaneous breathing throughout induction was considered foundational to safety. ‘Spontaneous respiration using intravenous anesthesia and high-flow nasal oxygen’ (STRIVE Hi) was successful in providing safe induction for the first described intubation of an adult TCS patient with hyperangulated blade ‘GlideScopeLoPro S4’ videolaryngoscopy.
TCS,Treacher Collins Syndrome; STRIVE Hi,SponTaneous Respiration using IntraVEnousanaesthesia and ‘Hi-flo’ nasal oxygen; LMA; Laryngeal Mask Airway, HFNO, High Flow Nasal Oxygen; TTH, The Townsville; Hospital CT, Computed Topography; ETT,EndoTracheal Tube; AFOI, Awake FiberOptic Intubation; BVM, Bag Valve Mask; TCI, Target-Controlled Infusion; Cp, Estimated ‘plasma’ site Concentration (of the Target-Controlled Infusion); Ce; Estimated ‘effect’ site Concentration (of the Target-Controlled Infusion); TIVA, Total IntraVenousAnaesthetic; POGO, Percentage Of Glottic Opening; CICO, Can’t Intubate Can’t Oxygenate; PEEP, Positive End Expiratory Pressure
Treacher Collins Syndrome is a disorder of the first and second branchial arches in neural crest formation.1 It is caused by a mutation on chromosome 5 and has an incidence of 1 in 40000-70000 births.2 The syndrome is characterised by symmetrical hypoplasia of the maxilla, mandible, and zygomatic process.3 These individuals are likely to present with a small oral aperture, abnormalities of the temporomandibular joint, retrognathia and palate deformities.3 These anatomical airway features create difficult intubating conditions4 which have been shown amongst pediatric patients to worsen with age.5
A comprehensive review of airway management amongst adult TCS patients does not exist – this is likely a reflection of the contemporary availability for pediatric corrective facial surgery.6 From the outset we considered caution in applying pediatric reviews towards adult patients, as airway features in syndromic patients inherently change with age.7
Previous adult TCS case reports have demonstrated difficulty with intubation and found success in backup second generation laryngeal mask airways (LMA).8,9 Paloma8used an LMA-Fastrach for an emergent caesarean section after blind intubation through the LMA was unsuccessful. An i-gel (Intersurgical Ltd., Wokingham, UK) was successfully used as backup for Soh9after two failed videolaryngoscopic, and two failed trans-nasal fiberoptic intubations attempts, for a 25-year-old male presenting for emergency bowel resection. To our knowledge, this case represents the first successful intubation of an adult TCS patient using hyperangulatedvideolaryngoscopy alone.
STRIVE Hi focuses on maintaining spontaneous ventilation and utilizing the advantages of high-flow nasal oxygen (HFNO) during general anesthesia. HFNO has gained traction within anesthesia with physiological benefits for spontaneously breathing patients including generation of positive airway pressure, increased FiO2, decreased ventilatory dead space and reduced upper airway resistance.10-12 Propofol has been the favored sole anesthetic agent for STRIVE Hi given its titratability and ability to suppress airway reflexes.13 Most recently this technique has demonstrated safety in surgical procedures upon structurally obstructed airway surgery14 and emergency intubation for a case of epiglottitis.15
This case presents the first described successful intubation of an adult TCS patient using STRIVE Hi and videolaryngoscopy. Written consent was granted by the patient for clinical photography and publication. Approval was sanctioned by the Townsville Hospital Health Service – Human Research and Ethics Committee. The applicable EQUATOR guidelines werereviewed.
A 76-year-old gentleman with Treacher Collins Syndrome was transferred to Townsville Hospital (TTH) with choledocholithiasis requiring an emergent open cholecystectomy and bile duct exploration. He previously presented to a regional hospital with epigastric pain and an obstructive liver function test profile. Computed topography (CT) scanning identified an obstructing 27mm suspected stone and common bile duct dilatation. He had remained hemodynamically stable and afebrile throughout. His past medical history contained hypertension and gastroesophageal reflux disease; he was effectively medically treated with amlodipine, perindopril, and esomeprazole. He had received one general anesthetic for a hernia operation greater than twenty years ago however no documentation was found. He lived alone, was completely independent and maintained an exercise tolerance greater than four metabolic equivalents. He abstained from both alcohol and tobacco. Upon review he was noted to have significant craniofacial dysmorphia: facial asymmetry, retrognathia, micrognathia, nasal bridge deformity and teeth agenesis (Figure 1). Ear malformations conferred lifelong conductive hearing deficit. His mouth opening was limited to two centimeters, thyromental distance was less than four centimeters and his range of neck motion was poor. The patient’s trachea and cricothyroid membrane were easily palpable. Examination identified no stigmata of systemic respiratory or cardiovascular disease.

Figure 1 Photos of the patient’s facial features.
These photographs demonstrate the patient’s dysmorphic airway features. Left image: front-on photo identifying nasal bridge deformity and teeth agenesis. Right image: side-on photo showing prominent retrognathia and micrognathia.
Written consent for images obtained in accordance with TTH Ethics Committee.
As this procedure represented open abdominal surgery with variable operating time, the optimal airway was an endotracheal tube (ETT). Given the expected difficulty of airway management, STRIVE Hi was chosen as the induction technique with a protocol previously described.14An airway plan was developed in consultation with the patient (Figure 2). The patient strongly preferenced STRIVE Hi over awake intubation methods.
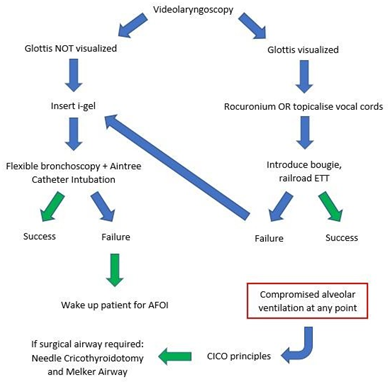
Figure 2 Flow diagram of airway plan following the possibilities of videolaryngoscopy.
Videolarnygoscopy “GlideScopeLoPro S4” (Verathon, Washington, USA); Intubating catheter “Aintree Catheter” (Cook Medical, Bloomington, Indiana); Second generation LMA “i-gel” (Intersurgical Ltd., Wokingham, UK); Cricothyroidotomy catheter “Melker Airway” (Cook Medical, Bloomington, Indiana).
AFOI, ‘Awake Fiber Optic Intubation’; BVM, ‘Bag Valve Mask’; CICO, ‘Cant Intubate Can’t Oxygenate’
Arriving to theatre a radial arterial line and two intravenous cannulae were inserted. HFNO (Optiflow THRIVE; Fisher and Paykel Healthcare) was introduced to the patient at 15L/min and titrated over three minutes to 50L/min. Glycopyrrolate 400mcg was provided intravenously as an antisialagogue and Co-Phenylcaine was administered to the oropharynx. Induction began with a propofol target-controlled infusion (TCI) using the Marsh-model at a plasma site (Cp) of 2 ug/mL. Once the difference between Cp and effect site (Ce) was less than or equal to 1 ug/mL, the Cpwas incrementally increased by 1 ug/mL. The patient lost consciousness at Ce 3 ug/mL. At this time, the HFNO flow was increased to 70L/min. Stepwise increase in Cp stopped at 6 ug/mL and Ce equilibrated. No opioid or other sedatives were co-administered. The patient maintained adequate spontaneous respiration with no airway adjuncts. A GlideScopeLoPro S4 laryngoscope (Verathon, Washington, USA) was introduced by the anesthetic fellow and identified a percentage of glotticopening (POGO) 100%. Lignocaine 1% topicalized the vocal cords and propofolCp increased to 8 ug/mL. The laryngoscope was removed and HFNO flow continued. After waiting 30 secondsthelaryngoscope was reintroduced, vocal cord view was reidentified, and a hyperangulatedbougie was passed between the cords. A size 8.0 ETT was railroaded into the trachea. Oxygen hemoglobin saturations did not fall below 98%, end tidal CO2 did not increase above 45mmhg and hemodynamic stability was preserved with small aliquots of metaraminol (2mg total). Remifentanil accompanied propofol to complete a total intravenous anaesthetic (TIVA). The propofol TCI was decreased to 4 ug/mL and the operation proceeded with no complication. Extubation was uneventful and he was discharged 3 days postoperatively.
In a previous case of unsuccessful intubation, authors discussed a narrow mouth opening (1.5 finger breadths) and small supraglottic area as the most significant anatomical features.9Similar facial features were present for our patient (mouth opening 2cm and profound retrognathia), influencing the use of the GlideScopeLoPro S4 videolaryngoscope. ‘GlideScope Spectrum Single-use’ are a range of videolaryngoscopes which include varying sizes of the hyperangulated low profile ‘LoPro’ and Macintosh ‘DirectView MAC’ styles. The LoPro in contrast to the MAC exaggerates blade angulation providing the best video view of the vocal cords achievable. Disadvantages include reliance on video view, difficulties with introducing the bougie, and occasional resistance passing the ETT around the axis of the oropharynx. Because of the degree of retrognathia and previously described difficulties by Soh9with a MAC blade, a LoPro was hypothesized as offering the best videolaryngoscopic attempt.
Fiberoptic trans-nasal intubation and LMA-intubation methods have demonstrated multiple successes among pediatric patients.4Trans-nasal intubation was potentially difficult due to unclear nasal anatomy but remained a secondary plan if trans-glotticvideolaryngoscopy intubation was unfeasible. Supported by success in previous case studies8,9ani-gel was readily available in the event of airway compromise. Prior experience of the lead anesthetist in performing emergency tracheostomies, together with an easily palpable cricothyroid membrane, influenced the choice of needle cricothyroidotomy and insertion of a Melker Airway (Cook Medical, Bloomington, Indiana) in the event of ‘Cant Intubate Cant Oxygenate’ (CICO).
Booth14demonstrated success with STRIVE Hi among 30 patients presenting for elective tubeless surgery upon severely obstructed airways. There were no episodes of oxygen desaturation, airway obstruction or apnea duringinduction. More recently STRIVE Hi was extended to safely intubate an adult patient with acute epiglottitis.15This featured a 54-year-old male who was stridorous with labored breathing and impending airway collapse, who was successfully intubated with a C-MAC videolaryngoscope, bougie and size 6.0 ETT. Lee15discussed the importance of familiarity with the process - avoiding apnea whilst achieving consistent end points for airway instrumentation. We strongly support this statement, that an anesthetist must be well versed in the process of STRIVE Hi in elective surgery settings, before extending it into airway emergencies or suspected difficult intubations. The safety of STRIVE Hi was demonstrated in our case, where an experienced approach facilitated safe videolaryngoscopy and subsequent intubation.
Intubating in the absence of muscle paralysis contributes a risk of sub-optimal glottic visualization, coughing and laryngospasm.15Given previously demonstrated difficulty of bag mask ventilation in patient with TCS,4 and therefore the likely difficulty in providing positive end expiratory pressure (PEEP), avoiding laryngospasm was a critical concern. On identifying a favorable view, the airway plan considered either direct vocal cord topicalization or muscle relaxation. The anesthetist was confident that thorough topicalization was possible. Together with an appropriate depth of propofol-induced anesthesia and oropharyngeal Co-Phenylcaine spray, maximal caution was taken short of muscle paralysis. Admittedly, given the favorability of the glottic view, overall risk between topicalizationor administering rocuronium is likely negligible. The intubating conditions would foreseeably only improve with muscle relaxation and Sugammadex (16mg/kg) was immediately available.
This case study seeks to build upon the sparse body of literature for intubation of adult Treacher Collins Syndrome (TCS) patients undergoing general anesthesia. It demonstrates a case of successful intubation with hyperangulatedvideolaryngoscopy. Pivotal to the safety of this procedure was maintaining spontaneous respiration whilst providing an adequate depth of anesthesia. This was achieved with STRIVE Hi, which safely maintained oxygenation and ventilation for our patient until the airway was secured.
Thank you to the Townsville Hospital Anaesthetics Department for your support during the production of this case report. In particular, the efforts of the coauthors for their reviews, critiques, and assistance throughout development.
The authors declare no conflicts of interest were involved in the production of this report.

©2020 Young, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.