Journal of
eISSN: 2373-633X


Case Report Volume 15 Issue 1
1Department of Internal Medicine, Corazon Locsin Memorial Medical Regional Hospital, Philippines
2Department of Pathology, Corazon Locsin Memorial Medical Regional Hospital, Philippines
3Department of Clinical Sciences, College of Medicine, University of St. La Salle, Philippines
Correspondence: Frederic Ivan L Ting, Department of Clinical Sciences, College of Medicine, University of St. La Salle, Philippines, Tel +63 34 434 6100
Received: December 29, 2023 | Published: January 19, 2024
Citation: Ababa RM, Ting KDR, Ting FI. Hepatocellular carcinoma presenting as a posterior thoracic mass: a case report. J Cancer Prev Curr Res. 2024;15(1):15-17. DOI: 10.15406/jcpcr.2024.15.00542
Liver cancer is the sixth most common cancer worldwide, and the fourth leading cause of cancer-related deaths. Among liver malignancies, hepatocellular carcinoma (HCC) is the most common and usually presents with abdominal pain. Although extrahepatic metastasis is seen in advanced stages, chest wall metastasis is extremely rare. This is a case of a 59 year old male, initially presenting with a superficial mass at the posterior thoracic area. Biopsy later revealed metastatic carcinoma from a liver primary. Computed tomography (CT) scan eventually revealed a mass at the right posterior chest wall and a nodule at the right hepatic lobe. This case report epitomizes the importance of proper and adequate biopsy and immunohistochemical staining to determine the primary site of malignancy which will ultimately determine the patient’s treatment approach and prognosis.
Keywords: thoracic mass, hepatocellular carcinoma, metastasis
Hepatocellular carcinoma (HCC) has the highest incidence rates in Asia due to the high prevalence of Hepatitis B virus (HBV) infection. It has a strong male predominance and is usually seen among 65-70 years old. The main risk factor is liver cirrhosis which is caused by chronic liver damage through inflammation and fibrosis either from chronic infection by HBV, Hepatitis C virus (HCV), alcohol abuse, or metabolic syndrome.1
The annual risk of HCC development is 3-8% in HBV or HCV infected cirrhotic patients. Ideally, ultrasonography every 6 months with or without serum α-fetoprotein (AFP) levels is the recommended method of surveillance for patients with risk factors of developing HCC. However, HCC is generally diagnosed at advanced stages in most Asian countries due to poor health seeking behavior and lack of surveillance. Patients are usually symptomatic at the time of consultation indicating an advanced stage with median life expectancy of <1 year.1
Extrahepatic metastasis of HCC is seen in advanced stages and are commonly found in the lungs (45-50%), abdominal lymph nodes (45%), bones (35-40%), and adrenals (12%). Chest wall metastasis is noted to be extremely rare since only a few cases have been reported.2 Thus, various diagnostic tests (imaging, biopsy, immunohistochemical stains among others) should be done to properly work-up and diagnose HCC with unusual presentations.3
This is a case of patient E.B., a 59 year old male who came in for consult due to a large palpable mass at the posterior thoracic area.
Fifteen (15) months prior to consult, the patient noted a soft, nontender, fixed nodule around 1 cm in size at the inferior posterior area of the thoracic wall. No other associated symptoms and no consult was done. In the interim, the mass further grew in size with intermittent mild tenderness. Ten (10) months prior to consultation, the patient went to the emergency room due to an enlarging very tender mass. A tissue biopsy of the thoracic mass was done revealing a poorly differentiated carcinoma (Figure 1). Immunohistochemical staining showed the following results: (+) HepPar1, (-) CK7 and (-) CK20, which are consistent with a diagnosis of hepatocellular carcinoma (Figures 2-4). The patient was also noted to be reactive to anti-HCV supporting the presence of Chronic Hepatitis C. A CT-scan was done showing a large (9.9 x 9.3 x 6.4 cm) homogenous mass at the right inferoposterior chest wall with osseous involvement with metastases to the lungs, bone, and a right hepatic nodule (2.1x1.9x1.9 cm) in segment 8 and segment 5 (Figures 5-7).
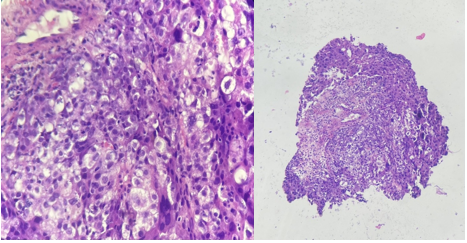
Figure 1 Histologic sections show fibrocollagenous to fibromuscular tissue fragments infiltrated by a malignant neoplasm arranged in solid sheets and lobule-like patterns. These malignant cells contain pleomorphic, hyperchromatic to vesicular nuclei with variably prominent nucleoli and moderate to abundant granular eosinophilic to vacuolated cytoplasm. Few mitotic figures are seen (0-4 mitotic figures per high power field) with some atypical forms.
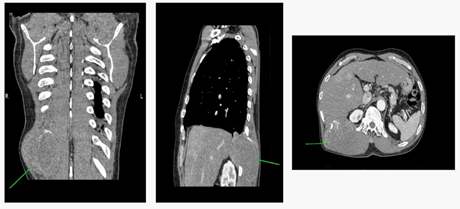
Figure 5 Coronal, sagittal, and axial view from left to right showing the 9.9 x 9.3 x 6.4 cm in homogeneously-enhancing, heterogeneous lesion with central hypodense areas in the right erector spinae muscle at the right inferoposterior chest wall. It is noted to extend into the right lower hemithorax with associated lysis of the 11th posterior rib. It displaces half of the right crus of the diaphragm anteriorly and abuts the posterosuperior portion (segment VII) of the right hepatic lobe.
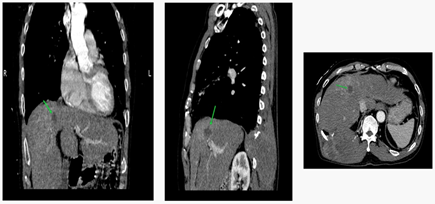
Figure 6 Coronal, sagittal, and axial view from left to right showing a 2.1x1.9x1.9 cm fairly-defined, ovoid, slightly enhancing, hypodense lesion at the segment 8 of the right hepatic lobe.
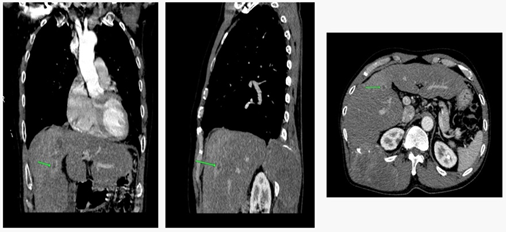
Figure 7 Coronal, sagittal, and axial view from left to right showing smaller, similar-looking lesions in the segment 5 of the right hepatic lobe.
The patient was lost to follow-up and the mass continued to grow with associated intermittent pain, significant weight loss of 15 kilograms in 4 months, and decrease in appetite. Increase in abdominal girth was also noted with no pain, changes in bowel movement or urination. Two (2) months prior to consult, severe pain was noted at the inferior posterior thoracic area radiating to the right upper abdomen. A palpable mass at the epigastric area around 3 cm in diameter was also noted. Persistence and worsening of symptoms eventually prompted the patient to seek consult.
On the day of consultation, the patient was noted to be ambulatory and having mild pain. The posterior thoracic mass was measured around 26 x 25 x 24 cm in size while the palpable epigastric mass was 4 x 4 x 5 cm (Figure 8). The patient was then advised for a repeat chest CT scan with contrast and laboratory tests in preparation for treatment planning.
Hepatocellular carcinoma (HCC) is a highly malignant tumor that can cause both intrahepatic and extrahepatic metastases. One-third of patients with HCC present with extrahepatic metastasis. The most common extrahepatic metastasis is commonly found in the lungs (45-50%), abdominal lymph nodes (45%), bones (35-40%), and adrenals (12%) while chest wall metastasis is extremely rare (<1%) with a poor prognosis.2-4
Biopsy is essential if hepatocellular carcinoma is found outside the liver and no primary focus is found within the liver. If no primary focus is found within the liver, the tissue biopsy must confirm the presence of normal liver tissue, including portal triads and cancer emboli within vessels near the tumor, for an accurate differential diagnosis.3 Our case initially presented with a palpable mass at the posterior thoracic area and biopsy of the said mass revealed a poorly differentiated carcinoma which for a time had an unknown primary site. In such cases, immunohistochemistry has become a crucial ancillary procedure in the identification and classification of carcinomas with unknown primary sites. Determining the primary site will have a major impact on prognosis and therapy.5
In the case presented, CK7 and CK20 immunohistochemical stains were utilized. Cytokeratins are intermediate filament proteins present in epithelial cells. They are expressed in a tissue-specific manner in normal organs and the tumors that arise from them. In a study done by Chu et al, they observed the following results: CK7 expression in the majority of lung, breast, endometrium, ovary, cervix, salivary gland, thyroid cancers, cholangiocarcinoma, and adenocarcinoma of the pancreas. On the other hand, CK20 was expressed in all colorectal adenocarcinomas and in the majority of gastric, pancreatic, and Merkel cell tumors. Prostate, kidney, and adrenocortical carcinomas as well as sarcomas, carcinoids, hepatocellular carcinomas and thymomas were negative for both CK7 and CK20 staining, while both stains were positive on many pancreatic and cholangiocarcinomas as well as some bladder and gastric tumors.6
Immunohistochemical staining done in the case presented revealed negative for both CK7 and CK20 staining, hence, HepPar 1 immunohistochemical stain was utilized in favor of Hepatocellular Carcinoma to which our case showed positive expression for the said stain. Data showed that HepPar 1 and AFP were good markers of extrahepatic metastases of HCC.7 Immunohistochemical demonstrations of HepPar1 and AFP were noted in 90% of HCC-confirmed tissue specimens in one study.8 A study showed that the sensitivity of ARG, GPC-3, HepPar-1, and AFP were 82.6%, 89.2%, 83.6% and 53.8%, and the specificity were 98.3%, 94.8%, 96.2% and 100%, respectively, suggesting that this panel be used to differentiate HCC from non-HCC especially in sites of extrahepatic metastases.9
Complete imaging studies should also be performed to properly determine the stage of malignancy.3 In this case, a CT-scan was done showing a large homogenous mass at the right inferoposterior chest wall with osseous involvement with metastases to the lungs and bone. A right hepatic nodule in segment 8 and segment 5 were likewise noted, consistent with the diagnosis of hepatocellular carcinoma based on the immunohistochemical [(+) HepPar1, (-) CK7 and (-) CK20] studies performed.
The stage of the tumor and the functional status of the liver determine the clinical presentation of HCC. The most common presentation of HCC is abdominal pain although some patients can be asymptomatic in the early stage of the disease especially those with no accompanying cirrhosis. On the other hand, patients with cirrhosis-related HCC may present with symptoms of decompensated liver failure, such as jaundice, hepatic encephalopathy, pruritus, ascites, palpable mass in the upper abdomen, fever, malaise, weight loss, early satiety, abdominal distension, and cachexia.4 Symptomatic patients may present with variceal bleeding, intraperitoneal bleeding, obstructive jaundice, and hepatic encephalopathy.7
For the management of HCC, several treatment options are available depending on the stage. For early stages, resection, liver transplantation, and local ablation have substantially improved life expectancy, with median overall survival (OS) times beyond 5 years. For intermediate stages, transarterial chemoembolization (TACE) has improved OS from 16 months (natural history) to 20–30 months. Finally, systemic drugs for advanced tumors (atezolizumab plus bevacizumab, sorafenib, lenvatinib, regorafenib, cabozantinib, and ramucirumab) have improved median survival times from 8 months to 19 months in the first-line setting and 10 months in the second-line setting.1
Primary prevention of HCC can be achieved by vaccination against HBV and effective treatment of HBV and HCV infection. Studies assessing the impact of universal vaccination against HBV infection have reported a significant decrease of the incidence of HCC. HBV vaccination is recommended to all newborns and high-risk groups, following World Health Organization guidelines. Vaccination is also recommended in people with risk factors for acquiring HBV infection, such as health workers, travelers to areas where HBV infection is prevalent, injection drug users, and people with multiple sex partners.1
Surveillance with ultrasonography every 6 months with or without serum α-fetoprotein (AFP) levels is recommended for cirrhotic patients due to various causes: those with HCV-related liver fibrosis, patients with chronic HBV infection, or a family history of HCC.
This case report epitomizes the importance of proper work-up and adequate biopsy and immunohistochemical staining to determine the primary site of malignancy which will ultimately determine the patient’s treatment approach and prognosis.
The authors would like to thank the patient and his family for consenting to this case report.
Authors declare that there is no conflict of interest.

©2024 Ababa, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.