Journal of
eISSN: 2373-633X


Review Article Volume 14 Issue 4
1General Surgeons, Assistants Surgical Clinic "A" Hospital de Clínicas Universidad de la República, Uruguay
2General Surgery Resident Physician, Hospital de Clínicas Universidad de la República, Uruguay
3Resident Physician of Vascular Surgery, Anatomy Assistant, Hospital de Clínicas Universidad de la República, Uruguay
4Endocrinologist, Associate Professor of Endocrinology and Metabolism, Hospital de Clínicas Universidad de la República, Uruguay
5General Surgeon, Prof. Attaché Surgical Clinic “A”, Hospital de Clínicas Universidad de la República, Uruguay
6General Surgeon. Prof. Director Surgical Clinic "A", Hospital de Clínicas Universidad de la República, Uruguay
Correspondence: Dr. Ulises Parada, General Surgeons, Assistants Surgical Clinic "A Hospital de Clínicas Universidad de la República, Ecuador 1648 Montevideo Uruguay, Tel 099313877
Received: August 12, 2023 | Published: August 23, 2023
Citation: Parada U, Fernandez L, Madera D, et al. Lateral neck lymph node dissection in papillary thyroid cancer: tactics and surgical technique. J Cancer Prev Curr Res. 2023;14(4):87-93. DOI: 10.15406/jcpcr.2023.14.00527
Failure of local control in a patient with advanced stage differentiated thyroid carcinoma is one of the main risks of recurrence and mortality. Therefore, the choice of surgical tactic plays a decisive role in obtaining a radical oncological resection. The lymph node dissection of the neck includes the resection of the lymph node and fascial cell tissue of the neck. The experience and training of the surgical team, as well as anatomical knowledge and a detailed surgical technique, are of invaluable importance to achieve the highest number of resected nodes with the least morbidity. The objective of the present work is to describe the surgical technique of cervical modified radical dissection (DRM) based on knowledge of the surgical anatomy of the neck, compartmentalization and the preferences of the author group.
Papillary thyroid cancer is the most common malignant tumor differentiated from follicular cells. Survival is measured at 10 years and is greater than 90%, which speaks of the indolent course of the disease. However, the recurrence of the disease reaches 30%.1,2 There are many factors that influence both survival and disease recurrence: age, pathological subtype, extension of the disease, incomplete resections, lymph node involvement.
Failure in locoregional control in a patient with advanced stage differentiated thyroid cancer is one of the main risks of recurrence and mortality. Therefore, the choice of surgical tactic plays a decisive role in obtaining a radical oncological resection. Lymph node dissection of the neck includes resection of the lymph node and fascial tissue of the neck.3 The experience and training of the surgical team are of invaluable importance to achieve the highest count of resected lymph nodes with the least morbidity.3,4 Multidisciplinary teamwork, such as that carried out in the Endocrine Surgery Unit of the Hospital de Clínicas (UCE), with a therapeutic management protocol, and a meticulous surgical technique constitute an essential part of the treatment and prognosis of CPT.
The objective of the present work is to describe the surgical technique of cervical modified radical dissection (DRM) based on knowledge of the surgical anatomy of the neck, compartmentalization and the preferences of the author group.
Topic limitation
Why differentiated papillary thyroid cancer?
We will focus on differentiated thyroid cancer (follicular and papillary) due to its frequency (90-95% of thyroid cancers) and within this, papillary carcinoma, since this is the one most associated with lymph node involvement.
What should the surgeon know?
The neck is essentially a passage region for structures that communicate the head with the thorax and upper limbs.
The number of contained anatomical structures (airway, vessels, nerves, thyroid) make this sector of the economy a relatively small surgical field with vital organs and others that without being vital, their injury would imply significant morbidity for the patient.
One of the most outstanding points of neck surgery is the identification of nervous structures, since their recognition is not easy and they are closely related to ganglionic groups. The challenge of cervical surgery to achieve oncological radicality and avoid sequelae lies in the precise anatomical knowledge of said region. Surgical anatomy divided by triangles (Figure 1).
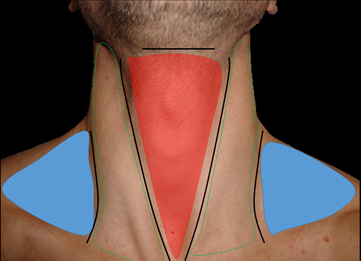
Figure 1 Surgical anatomy: division by triangles.
Red: Anterior triangle with inferior apex, medial to the ECM (Infra Hioidea region)
Skin: Triangle of the ECM with the upper apex (carotid region)
Celeste: Posterior triangle with apex towards the outside (between the ECM and the trapeze, external supraclavicular region).
Anterior triangle of the neck (infrahyoid region of the "classics")
Boundaries:
Superior: hyoid
Lateral: leading edge of ECMs
Bottom: sternal notch.
Posterior or deep: prevertebral fascia and prevertebral muscles
Content: Thyroid gland, parathyroid gland, visceral axis, cervical ganglion sympathetic chain.
Carotid or ECM triangle
Boundaries:
Superior or vertex: mastoid process
Bottom: ECM clavicular insertion
Sides: Both edges of the ECM
Content: primitive carotid artery, carotid bifurcation, internal carotid, external carotid and collateral branches (superior thyroid, posterior auricular, occipital, ascending pharyngeal, lingual, facial, external maxilla) and terminals (superficial temporal and internal maxillary), internal jugular vein and tributaries (pharyngeal vein, superior thyroid vein), vagus nerve, spinal accessory nerve, hypoglossal, hypoglossal loop, part of cervical sympathetic trunk.
Posterior triangle of the neck
Boundaries:
Bottom: clavicle
Anterior: Lateral or trailing edge of the ECM
Posterior: anterior border of the trapezius
Content: Spinal accessory nerve, a portion of the internal jugular vein near the origin, subclavian vein, subclavian artery, deep cervical plexus nerves, primary trunks of the brachial plexus, phrenic nerve, lymph nodes.
The three aforementioned regions are circumscribed by three concentric musculoaponeurotic planes with respect to the cervical spine.
The first plane is given by the superficial lamina of the cervical fascia or superficial cervical aponeurosis that surrounds the ECM muscles in front and trapezius muscles in posterior. The second plane is given by the pretracheal plate or median cervical aponeurosis, which contains the infrahyoid muscles. The third plane is made up of the prevertebral lamina or deep cervical aponeurosis, containing the prevertebral muscles.
Between the two first planes and the last one, there is a space, called by some authors as the visceral compartment of the neck that contains the visceral axis of the neck given by the laryngotracheal ducts to the anterior, pharyngoesophageal ducts to the posterior, thyroid gland in front and on the sides of the trachea, and various neurovascular elements to highlight the carotid jugulo axis surrounded by the carotid sheath. The so-called neurovascular bundle of the neck is made up of the internal jugular vein, the primitive carotid artery, and the pneumogastric nerve.
Neck nerve anatomy
The head and neck are innervated by the cranial nerves, the cervical plexus, the brachial plexus, the posterior rami of the cervical nerves, and the cervicocephalic portion of the sympathetic trunk. Certain cranial nerves and nerves of importance in the neck are described since these acquire a close relationship with the ganglionic groups:
The cervical lymph nodes range from 150–300 and represent 1/3 of the total, which makes the neck a region with the largest number of nodes. To understand it, it is necessary to divide the neck into ganglion levels.
Lymph node compartments of the neck (Figure 2):
|
Node |
Level |
|
I |
Submental (Ia) and submandibular (Ib) |
|
II |
High carotid jugular: from the base of the skull to the hyoid bone and from the stylohyoid muscle to the posterior edge of the sternocleidomastoid muscle (ECM). Anterior to the spinal nerve (IIa); behind the spinal nerve (IIb) |
|
III |
Medial carotid jugulum, located between the hyoid bone and the lower edge of the cricoid cartilage; the anterior and posterior border are the anterior and posterior border of the ECM muscle. |
|
IV |
Low carotid jugulum, between the lower edge of the cricoid cartilage and the clavicle; its borders correspond to the ECM muscle. |
|
V |
Supraclavicular, from the posterior edge of the ECM to the trapezius muscle and from the mastoid process to the clavicle; It is subdivided into Va nodes above the plane that passes through the lower edge of the anterior cricoid ring and Vb nodes located below said plane, as shown in the figure. |
|
VI |
Lateral limit, carotid arteries above and the hyoid bone below the sternal manubrium. |
|
VII |
Cervico-mediastinal (or antero-superior mediastinum) |
The objectives in neck lymph node dissection may be:
The modified radical lateral dissection in the CPT is indicated in those patients who present adenopathies that are palpable or detectable by ultrasound (in compartments II-V) with FNA compatible with metastatic disease or in the intraoperative examination with a positive extemporaneous biopsy. From the above, it can be deduced that the indication for DRM in CPT is therapeutic or rescue, but not prophylactic.
Surgery at the cervical level has undergone changes throughout its history, since 1906 with Crile considered "father of radical dissection" where the internal jugular vein (IVY), sternocleidomastoid muscle (ECM) and spinal nerve were resected in addition to the ganglionic groups. (NE), often with the sole objective of improving the surgical field.7 Until then, the concept of the time was followed: “the more, the better”. Over the years, this last concept began to be questioned and lost supporters, largely supported by the morbidity it generated (dropped shoulder, winged scapula, face edema).
Based on anatomical and pathological knowledge, the concept is changed to en bloc, compartmentalized and functional surgery (preserving VYI, ECM and NE). Added to this is the use of better technology such as magnifying glasses, coagulation materials, more precise instruments, and intraoperative monitoring of the recurrent laryngeal nerve. In this way we managed to preserve the oncological radicality and therefore survival, decreasing morbidity.
Classification of lymph node dissections
In 2002, the American Academy of Otolaryngology-Head and Neck Surgery proposed a standardized classification system to name the various neck dissections that are still in use today.5,8-10
DRM of the neck is classified as type I, II or III according to the structures that are spared during surgery.11
General concepts
For practical reasons and because it is considered the gold standard technique for the locoregional control of CDT, we will focus on the description of DRM.
The lymph node dissection of the neck must be based on the lymph node compartments, which have precise anatomical limits and this constitutes the basis of cervical cancer surgery. From what has been said, the picking technique or technique of gathering berries is formally contraindicated.
In the presence of confirmed lymph node metastases in the lateral compartment, emptying the latter and the central compartment is recommended, even if the latter is free of obvious involvement.
Prophylactic emptying of the lateral cervical compartment in the CDT (levels II to V) is not indicated in any case.
Before starting surgery, coordination between the surgeon and the pathologist is recommended to obtain the best technical performance. The conditions for sending material and clinical information are proportional to the quality and detail of the anatomopathological reports.
Making anatomical drawings or diagrams of lymph node areas can improve communication and obtain the highest diagnostic accuracy after the patient.
Contraindications
Absolute: Unrespectable disease due to compromise of the base of the skull and the deep muscles of the neck. Involvement of the carotid artery can be considered an absolute or relative contraindication. Extremely rare to see on CDT.
Lymph node resection of the neck presents relative contraindications such as uncompensated coagulopathies, general comorbidities with high surgical anesthetic risk, and the patient's cognitive status. In any case, it is the surgeon's judgment that must consider (after correctly assessing the patient) whether or not surgery is indicated.
Materials
It is necessary to have precision surgical material to perform a meticulous technique. We prefer the use of vascular surgical material that allows optimal handling of the delicate cervical anatomy (dissecting forceps, scissors, vessel loop, delicate thread guide).
Vascular sealants, both harmonic scalpel and ligasure, are very useful when dissecting lymph node structures, expedite surgical time and allow good hemostasis while maintaining a bloodless surgical field (a fundamental condition to avoid nerve injuries). If necessary, we use polyglactin 910 or a clipper.
Material's list
Patient preparation
In principle, it is a clean surgery, which is why some authors prefer not to carry out antibiotic treatment. The possibilities of opening the airway and digestive tract (rare event) would lead to contamination of the area. However, the large dissection involved, as well as the operating time, presence of dead space and drainage, makes it preferable to perform Cefazolin 2 grams i/v 30 minutes before surgery in a prophylactic way.
Patient position
It is placed in dorsal decubitus, with neck extension, always taking care not to hyperextend it, avoiding injuries, especially in those patients with a history of previous cervical pathology. It is useful to place an interscapular camber to achieve a good position and surgical field, it exposes the gland better and in the case of having an intrathoracic extension, the extension of the neck decreases the intrathoracic component (it raises the gland and makes it more superficial), making it easier to dissection.
At the cephalic level, putting together a donut or crown-shaped dressing that allows a good position and exposure to be achieved, fixing the patient's head can also prevent intraoperative extubation.
As regards the emptying time itself, the patient should be in supine position, with an extended neck, lateralized to the opposite side to the side of the dissection. We must have a correct exposure of the area, with a good visual of the anatomical representations. The lower lip and earlobe will be exposed, up to the clavicle; and from the trapezius and the ear behind to the midline.
Alcoholic chlorhexidine may be used as an antiseptic. The placement of the fields consists of a double field: at the cephalic level in a triangular shape, the most superficial one that surrounds the head and the lower square or rectangular one covers the table.
A slight elevation of the head by moving the operating table in an anti-Trendelemburg manner improves venous drainage from the neck.
Incision
The choice of type of incision in surgery is of great importance since it must allow us to approach all the lymph node regions to obtain good oncological results. At the same time, we must add obtaining cosmetic results and correctly vascularized flaps to avoid necrosis. It is recommended that the marking of the incision be carried out with the patient awake in anatomical position, preventing the anatomical reperes from being lost following skin folds.
There are multiple incisions as shown in Figure 3.

Figure 3 Neck incision according to biotype.
Paul André incision in hockey stick or J in long necks.
Kocher incision in short necks.
When defining the type of incision, it is necessary to be clear about the characteristics of the neck:
For patients with long necks, we prefer the hockey stick, Paul André or “J” incision behind the ECM muscle, which allows us to correctly approach the supraclavicular nodes and the high jugulocarotid region.
Another advantage of this type of incision:
In those patients with brevilinear or normal necks, we can reach the highest jugulocarotid sectors, as well as supraclavicular sectors, by means of a wider Kocher incision (making flaps). This type of incision has been the traditional approach to thyroid surgery since the late 19th century and is well known to all surgeons. In cases of lymph node dissection, it is necessary to create more extensive flaps, especially to allow us to reach the high carotid groups. If it is not possible to reach them, a technical "trick" is to make a small distal curvature towards the cephalic sector for better access to group II.
Although the other incisions allow the correct dissection of the lymph node groups, many are unsightly, deforming, or can even expose the neck vessels in case of infection or necrosis.
Regardless of the incision made, the flaps are raised below the plane of the platysma, with the necessary depth so as not to compromise its vascularization, thus avoiding necrosis. It can be performed with a monopolar or even cold scalpel, since it is an avascular plane. The upper flap is released to the lower border of the mandible and the lower flap to the upper border of the sternoclavicular border. It is up to the surgeon's preference to sew compresses to the fields or not; the authors prefer this procedure since it allows us a wide field, the second assistant remains "free" to better expose the anatomical structures of the region, especially the ECM muscle, which, as we will see later, plays a fundamental role in exposing the lymph nodes. The carotid jugulo chain. Another advantage is the fact of isolating ourselves in contact with the skin. The disadvantage lies in the time that this procedure takes, although once the team gets used to it, it does not take more than a few minutes.
The section of the skin and the subcutaneous cell in the formation of the flaps carries with it superficial branches of the cervical plexus and the section of the external jugular vein. The region should be exposed: the clavicle below, the lower edge of the jaw above, the midline of the neck on the inside, and the edge of the trapezium on the outside.
Dissection
The strategy adopted by the author group is to carry out a dissection that begins at the supraclavicular level, taking all the cellulolymphatic and adipose tissue from the bottom up and from the outside in.
ECM muscle dissection
Once the subplatimal flaps have been carved, we must begin to expose the limits of the dissection (Figure 4).
Superior: lower border of the mandible
Medial: midline
Bottom: clavicle
Posterior: trapezius muscle
The dissection of the ECM begins with ligation of the external jugular vein followed by a longitudinal incision along the posterior edge dissecting the superficial fascia. The critical sector in the dissection is located in the upper half of the muscle, more precisely at the junction of the upper 1/3 with the middle 1/3. At this level the spinal nerve (SP) enters the ECM. The transverse process of the atlas serves as an anatomical reference when identifying it. Once the ECM has been dissected, it is useful to load it using a vessel loop that allows it to be separated from the deep planes and mobilized laterally and medially during the dissection of the cellulolymphatic and adipose tissue.
Dissection of the supraclavicular region (Figure 4)
Once the ECM is loaded, the dissection begins in the direction described above from the anterior edge of the trapezium and above the clavicle we will advance in the direction of the ECM. The branches of the brachial plexus that come out between the anterior and middle scalenes must be identified and not injured, as well as the phrenic nerve in front of the anterior scalene. The structures to take into account so as not to injure so far would be: NE, brachial plexus, phrenic nerve, internal jugular, and carotid artery. The dissection that is carried out close to the nervous elements requires great care, especially when using an electric scalpel due to heat dissipation, so the use of ligasure is preferred, remembering that although heat dissipation is less, it exists and the risk of injury therefore present. Maintaining a superficial plane to the scalene fascia (deep layer of the cervical fascia) is the preferred technique of the author group to avoid injuring the brachial plexus and the phrenic nerve.

Figure 4 Post emptying view of cellulo-lymphatic tissue in the supraclavicular hole and lower carotid region.
(ECM); Sternocleidomastoid muscle, loaded with vessel loop moved medially. (MEA); anterior scalene muscle.
(CT); thoracic duct, leading to Pirogoff's yugulosubclavian angle. (PB); branches of the brachial plexus.
Spinal nerve dissection
One of the most important steps is the identification of the spinal nerve (SP) since its lesion carries negative connotations since it is a motor and sensitive nerve. It is found in the cervical soft tissue and not the facial one; part of the retrostylus region is related to the internal jugular vein, then to the deep face of the ECM muscle, to later emerge in the supraclavicular region.
Once identified, it is loaded with a vessel loop (avoiding traction so as not to injure it), in this way we have it in sight and we protect it throughout its journey and dissection. The resection piece must be separated from the NE and released from the posterior face of the ECM, pulling the latter towards the zenith. Once separated, the retromuscular passage of the piece from lateral to medial is performed.
Dissection of the jugulocarotid region (Figure 5)
Upon reaching the ECM previously loaded with the vessel loop, it can be pulled toward the zenith and medially to resect the cellulolymphoid and adipose tissue of the lower and middle jugulocarotid region; then towards the zenith and lateral, to finish addressing the middle and upper carotid jugulo region. In this step of the carotid dissection we take into account the jugulosubclavian confluence; on the left side the thoracic duct and on the right the right lymphatic duct. These structures mark the limit of the dissection and must be preserved. Most of the time, detachment of the ECM muscle is not necessary, but in the case of large adenopathies, it can be sectioned and give excellent exposure and fixed again without leaving major sequelae.

Figure 5 Carotid region right side view (A) and left side view (B): Yugular vein load (VY), lateral retraction of the sternocleidomastoid muscle (SCM), Thyrolinguofacial trunk (TRLF) and hypoglossal nerve (NH).
Dissection of the submandibular triangle
Corresponds to the resection of the submental and submandibular lymph nodes. Resection of the submandibular and parotid gland is not necessary. We incise the fascia below the edge of these glands preserving the marginal branch of the facial nerve. Dissection continues through the digastric and stylohyoid muscle. These muscles retract and allow superior jugular and subdigastric access.
The hypoglossal nerve is identified inferior to the medial tendon of the digastric muscle. The lingual vein can be seen crossing the nerve superficially. Emptying continues as the upper limit of the crossing of the hypoglossal muscle and the posterior belly of the digastric muscle; nodes above these reperes are rare in CDTs. In addition, the NE can be injured. The surgical piece is retracted inferiorly to the previously dissected sector, obtaining a complete resection piece.
Sending the sample for an anatomopathological study is of great importance and must be part of the technique. To do this, a scheme is made in the study request with the regions sent repaired and numbered, if possible as a single piece. Otherwise, each bottle must be correctly labeled with the lymph node group it represents. The pieces must be labeled at the moment they are resected, in this way confusion and forgetfulness are avoided (See Figure 1).
It is necessary that pathology colleagues have an easy understanding of the material sent in a simple and practical way, since they are ultimately the auditors of the surgery performed. Once the piece has been extracted, it is necessary to carry out an exploration of the area, for this we will carry out a wash with warm physiological saline, (not cold) in order to remove the devitalized tissue and not attack noble structures such as nerves and parathyroid glands.
No effort should be spared in performing a correct haemostasis of the area; Today we have many hemostatic agents, harmonic, ligasure, monopolar, the important thing is to remember their heat transfer to a greater or lesser extent, which can cause injuries due to heat dissipation. Ligation with polyglactin 910 4 or 5–0 is preferable in regions close to or in nerve contact.
Leaving a drain is, in the opinion of the author group, essential, for some practical reasons, on the one hand, because the great lymphatic emptying entails an important sero-hemato-lymphatic drainage, which can last for 3 or 4 days. The presence of bleeding can alert us to a possible complication such as asphyxic neck hematoma.
Although there are several drainage modalities, the authors use a suction system that allows us to: keep the wound dry, simultaneously draining the lateral cell-lymphoganglionar surgical bed, and eventually central, avoiding the formation of collections.
The choice of drainage is not minor, it must not be too small as it is easily covered, it must be soft, silicone-coated and it must not be in direct contact with vessels in the neck. It is removed by contra-opening and fixed to the skin. We perform intradermal stitches in continuous suture skin.
It is recommended to use vessel sealants throughout the dissection because this makes it possible to expedite surgery as long as its use is meticulous and away from noble structures. In areas close to nerves and/or vascular structures, both the use of ligation with restorable materials and metal clips can be helpful.
The lymph node count according to the international bibliography should be above 20 nodes in unilateral modified radical neck dissection.12 The systematization and protocolization of both therapeutic management and surgical techniques are the basis for improving results.
None.
Authors declare that there is no conflict of interest.

©2023 Parada, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.
 Month of May is here, which is commonly known as the World Skin cancer awareness month, The major aim of this program is to Educate people on multiple ways on the prevention. To be part of this, we are doing our best to spread its awareness by accepting articles on this topic and grab best discount of 30% for your submissions to our Journal of Cancer Prevention & Current Research (JCPCR).
Month of May is here, which is commonly known as the World Skin cancer awareness month, The major aim of this program is to Educate people on multiple ways on the prevention. To be part of this, we are doing our best to spread its awareness by accepting articles on this topic and grab best discount of 30% for your submissions to our Journal of Cancer Prevention & Current Research (JCPCR).