Journal of
eISSN: 2373-633X


Research Article Volume 14 Issue 6
1Assistant Surgeon Clinical Surgical Clinic "A" Hospital de Clínicas, Uruguay
2Resid. Clinical Surgical Surgery "A" Hospital de Clínicas, Uruguay
3Adj. Prof. Clinical Surgical Surgery "A" Hospital de Clínicas, Uruguay
4Chief of Head and Neck Oncological Surgery Division, Hospital de Clínicas, Argentina
5Prof. Clinical Surgical Surgery "A" Hospital de Clínicas, Uruguay
Correspondence: Ulises Parada, Assistant Surgeon Clinical Surgical Clinic "A" Hospital de Clínicas, Ecuador 1648 Montevideo Uruguay, Tel 099313877
Received: November 02, 2023 | Published: November 27, 2023
Citation: Parada U, Guarneri C, Fernandez L, et al. Mini-incision surgery for hyperparathyroidism: first experience of the endocrine surgery unit of a university center in Montevideo. J Cancer Prev Curr Res. 2023;14(6):126-130. DOI: 10.15406/jcpcr.2023.14.00535
Introduction: Hyperparathyroidism (HPT) is the increased secretion of parathyroid hormone (PTH) from the parathyroid glands (GP). Surgical treatment remains the only one capable of curing the disease in primary hyperparathyroidism (PHP) as medical management eventually fails. In secondary hyperparathyroidism (SHP), parathyroidectomy allows control of hypercalcemia levels and its adverse effects. The trend in surgery is to perform less and less invasive approaches offering similar or better results to conventional surgery. The mini-incision surgery in which we focus our work is defined as the performance of a 1.5-2.0 cm transverse incision in the anterior face of the neck.
Objective: To evaluate the therapeutic results of the neck-centered mini-incision approach applicable to primary and secondary hyperparathyroidism. To show the casuistry of the mini-incision approach in patients with primary and secondary hyperparathyroidism in a Mutual and University center of Montevideo.
Material and methods: Observational, descriptive and retrospective study. A sample of 43 patients was studied. The database was obtained from the electronic registry of surgical coordination for a period of 5 years, after which the corresponding electronic medical records were reviewed.
Conclusions: The mini-incision approach can be applied to both primary and secondary hyperparathyroidism. It is a safe procedure, being successful in 90% of the cases in our casuistry. The directed and minimal dissection of the tissues is the basis for not having adverse effects in this series of cases, such as recurrent laryngeal nerve injury and neck hematomas. It also fulfills aesthetic objectives: small and symmetrical wound on skin fold.
Hyperparathyroidism (HPT) is defined as increased secretion of parathyroid hormone (PTH) from the parathyroid glands (GP).
Two clinical forms are distinguished according to their etiology:
The diagnosis of hyperparathyroidism is purely biochemical and does not require imaging. Surgical treatment remains the only one capable of curing the disease in PPH as medical management ultimately fails. In HPS, parathyroidectomy allows control of hypercalcemia levels and its adverse effects. The trend in surgery is to perform increasingly less invasive approaches offering similar or better results to conventional surgery. There are studies that show that in PPH the mini-incision approach and bilateral neck exploration have similar results in terms of therapeutic success and the appearance of adverse symptoms.1 For this purpose, pre- and intraoperative imaging techniques are used to topography the lesion as well as the analysis of intraoperative parathyroid hormone (PTHIO).2,3
The use of pre- and intraoperative technology makes it possible to identify the pathological gland and perform an approach without the need to explore other territories, thus leaving untouched sectors of the thyroid lodge. In the case of HPS, the mini-incision allows direct access to the GPs and reduces not only the size of the incision but also the dissection of the tissues, without forgetting that these are usually necks with multiple surgical approaches.
The mini-incision surgery on which we focus our work is defined as the performance of a 1.5-2 cm transverse incision in the anterior face of the neck, in such a way as to allow a directed and focused exploration.4 Percutaneous treatment by radiofrequency ablation, especially in PPH, can be considered as a therapeutic alternative in selected cases.5 Robotic surgery adds increased time, complexity, and cost.6
Target
To evaluate the therapeutic results of the neck-centered mini-incision approach applicable to primary and secondary hyperparathyroidism. To present the casuistry of the mini-incision approach in patients with primary and secondary hyperparathyroidism performed by members of the Endocrine Surgery Unit in 2 centers in Montevideo (Mutual and Universitario).
Observational, descriptive and retrospective study. The database was obtained from the electronic registry of surgical coordination in the period established between October 2018 to October 2022, after which the corresponding electronic medical records were reviewed. The information obtained focused on age, sex, years of evolution, clinical, associated thyroid pathology, pre and postoperative values of PTH, calcemia and ionic calcium, preoperative and intraoperative imaging studies, topography of the affected gland or glands, operative time, hospital stay, postoperative complications and pathological anatomy.
Inclusion and exclusion criteria were established as shown in Table 1. Preoperative imaging assessment was performed by one or more methods to certify and topographically identify the affected gland or glands.
Inclusion criteria |
Image identification of one or more lesions |
Lesion with neck topography |
No previous intervention in thyroid loggia |
Exclusion criteria |
Family history of MEN |
Under 18 years of age |
Table 1 Inclusion and exclusion criteria
Regarding the surgical technique: general anesthesia was performed in all cases, with outpatient hospitalization in cases of PPH and hospitalization for management of the internal environment in cases of HPS (Table 2, 3).
|
PPH: Advantages of the mini-incision approach |
|
⦁ Limited and focused dissection of the affected GP |
|
⦁ Indemnity of the contralateral lodge |
|
⦁ Short-term surgery |
|
⦁ Easily controlled pain |
|
⦁ Allows bilateral scanning |
|
⦁ Better aesthetic results |
|
⦁ Outpatient surgery |
|
⦁ Comparable results with respect to the traditional approach |
Table 2 Advantages of the mini-incision in the PPH approach
|
HPS: Advantages of the mini-incision approach |
|
⦁ Limited and focused dissection of the affected GPs. |
|
⦁ Targeted approach avoids previously operated areas (vascular accesses). |
|
⦁ Less tissue dissection and therefore less risk of bleeding and recurrential injury. |
|
⦁ Improved aesthetic result |
|
⦁ Easily controlled pain |
|
⦁ Allows bilateral scanning |
|
⦁ Comparable results with respect to the traditional approach |
Table 3 Advantages of the mini-incision in the HPS approach
Prior to the start of surgery we performed a blood extraction to measure PTHIO, which will be compared with the figures after the extraction of pathological parathyroid glands. Once the patient has been intubated and placed in its final position for surgery (neck extension), an ultrasound was performed to accurately topography the parathyroid gland or glands and proceed to its marking at skin level (Figure 1A, B and C).

Figure 1 A, Preoperative ultrasound; B, Ultrasound identification of parathyroid glands; C, Ultrasound marking of glandular topography; D, Mini incision.
A 1.5 to 2 cm long incision centered in the neck was made over the skin fold in order to be more esthetic (Figure 1D). Due to the laxity of the skin it is possible to move this incision to the topography of the glands. This allowed direct access both to the superior glands between the superior thyroid artery and the recurrent laryngeal nerve, and to the inferior glands behind the inferior thyroid pole. Once identified (Figure 2A) it is resected and sent for anatomopathological study. In the case of HPS, after identifying the 4 glands, we performed a 7/8 parathyroidectomy leaving the GP in situ marked with a metal clip. The GP of choice to preserve its half was the one we identified with the least macroscopic alteration related to its size (preservation of the smallest one). After 10 minutes after the last pathological GP was removed, a sample was taken for PTH. Using Miami criteria, PTH must decrease at least 50% of its initial value to be considered a successful parathyroidectomy in PPH.1 In HPS a decrease of 70% is expected.
Indocyanine green has been a recent acquisition in our environment so it is not yet available for all patients, reserving its use in cases of HPS. In the patients in whom Indocyanine green marking was used intraoperatively (all HPS, 19 cases), it was helpful in the identification and dissection of the GPs. It also allows predicting with certainty the viability of the parathyroid remnant and its functionality, since its vascularization and therefore its function is proportional to the degree of glandular fluorescence (Figure 2B).
In all cases we had magnification with the use of magnifying glasses, electric scalpel, ligasure, vascular surgery material, metal clips. The resected GPs were sent for extemporaneous anatomopathological study. No systematic search or monitoring of the recurrent laryngeal nerve was performed intraoperatively. No glove sheet or other types of drains were used in the surgical site. Closure was performed with 4-0 monocryl intradermal continuous stitch (Figure 2C).
A sample of 43 patients with PTH was studied. Of which 24 patients (55.8%) corresponded to PPH and 19 patients (44.2%) to SPH (Figure 3A).
The surgical indication arose in each case from a multidisciplinary meeting in the context of the Endocrine Surgery Unit, not being the m isma object of study in the present work. A percentage of the patients were asymptomatic, the rest presented renal lithiasis and/or osteoporosis.
Regarding HPPs
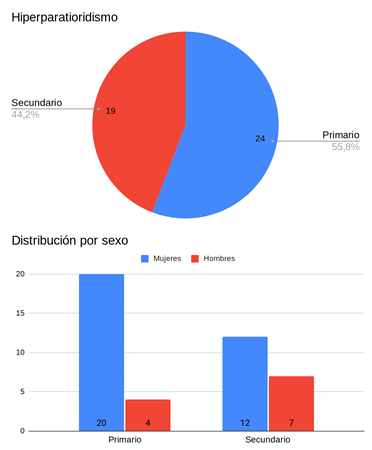
Figure 3 A, Percentage of primary and secondary hyperparathyroidism; B, Distribution of HPT according to sex.
The average time of evolution of the disease was 15 months.
Regarding HPS
Like many other surgical techniques, parathyroidectomy has evolved since its first description in 1925 to date. The traditional technique consists of a transverse neck incision of no less than 3 cm (Kocher) and exploration of the 4 glands. It was the only one available before the development of imaging and laboratory techniques.
Today a small approach no larger than 2.0 cm can be performed allowing direct access to the affected GPs (focused parathyroidectomy) by performing a limited dissection, without making a deliberate attempt to dissect the normal GP. These changes are undoubtedly the result of technological advances that allow preoperative identification with scintigraphy with Tc 99 sesta MIBI combined with SPECT-CT and preoperative ultrasound. These studies make it possible to plan the surgery and are the basis of the mini-incision approach. The success of the surgical procedure is confirmed with intraoperative PTH (PTHIO) and extemporaneous and definitive anatomopathological study. The short half-life of PTH ranging from 3 to 5 minutes has made intraoperative monitoring a useful adjunct to parathyroid surgery. Routine use of PTHIO in focused parathyroidectomy offers reassurance to the patient and surgeon by ensuring removal of all hyperfunctioning glands.9 In the event that the PTHIO does not drop sufficiently we must continue the exploration.
The diagnostic accuracy of ultrasound and scintigraphy with Tc 99 sestaMIBI combined with SPECT-CT is similar and is around 90% and when these methods are combined the localization accuracy increases above 95%. However, 4-D computed tomography seems to have greater diagnostic sensitivity than ultrasound and Tc 99 scintigraphy.10 In the present study, ultrasound detected 70.8% of the GPs, a figure somewhat below the reference center values of around 90%. The scintigraphy with Tc 99 sestaMIBI combined with SPECT-CT on the other hand detected 87%, close to figures in reference centers of 91%. The two methods added together increase sensitivity, reaching figures of 95.6%.11,12
Undoubtedly the greatest advantage of focused exploration is seen in PPH as can be seen in the literature, which highlights the performance of outpatient surgery and the indemnity of the contralateral loggia. Most of the time it is a short duration surgery, with minimal tissue dissection, which makes pain easily controllable. Preoperative identification of a single lesion allows dissection of the affected gland without the need for exploration of the contralateral side, ensuring the viability of at least 2 GPs, which assures us in part, a good management of calcium metabolism avoiding hypocalcemia.
When the neck is approached by mini-incision, exploration of the contralateral side is possible due to the laxity of the skin at the neck level. Although a small incision could make dissection and vision difficult, the use of vascular surgery material, precision, magnification with a magnifying glass and a correct knowledge of the surgical anatomy of the region allows this possible "disadvantage" to be easily overcome. Furthermore, GP surgery is ideal for this approach because 85% of the lesions are single lesions, it is an anatomical surgery that does not require large reconstructions and most of the lesions are small in size (1 to 2 cm). Table 2 summarizes the advantages of the mini-incision approach for PPH.
In HPS, 7/8 parathyroidectomy is a reasonable option in patients with CKD refractory to medical treatment, achieving a decrease in mortality. This normalizes calcium and phosphorus, decreases the rate of fractures and improves quality of life.13 Parathyroidectomy performed before renal transplantation was even associated with a lower risk of graft failure.14,15
With respect to HPS and the mini-incision approach, the situation is different from that of PPH. The benefits do not seem to be so clear at first sight (bilateral exploration required). However, many of the advantages can be extrapolated to HPS. The fact of using a mini-incision approach does not rule out the exploration of the 4 GPs.
In the chronic renal patient with HPS, the presence of concomitant conditions such as coagulopathy, immunosuppression and multiple interventions at the cervical level by vascular approaches stands out, which results in an increase of locoregional comorbidity. This is why a targeted approach, with minimal tissue dissection, is key to reduce the risk of bleeding, avoid previously intervened areas and thus mitigate the possibility of recurrent laryngeal nerve injury. Table 3 summarizes the advantages of the mini-incision approach for HPS.
The most important limitation for the mini-neck approach is the possibility of ectopic and supernumerary glands (especially those far from the cervical region). This eventuality is considered a diagnostic and therapeutic challenge.
According to the results of recent studies, a reduction of 60% or more in IOPTH at 10 min after parathyroidectomy has an accuracy of 94.4% and a positive predictive value of 100%.16 Intraoperative monitoring is very useful to measure the success of the procedure, however there is no single concept of a "cure" for HPS since in many cases, regardless of the decrease in IOPTH, the definitive normal range is not reached.9
There is evidence that mini-incision surgery in PPH is a safe technique, reduces operative time, complications and hospital stay when compared to bilateral neck exploration with similar cure rates.17-19 Parathyroidectomy in HPS is usually performed through a Kocher incision,20 although there are reports of minimally invasive approaches.21,22
Although there are no communications that propose resolution by a small, single, skin-centered approach for HPS, we believe that the benefits of this approach can be extrapolated. Immediate preoperative marking by ultrasound and the use of indocyanine green allows identification of the 4 glands making the mini-incision approach feasible and safe. We have had no complications related to the surgical technique. It should be noted that morbidity related to recurrent laryngeal nerve damage and hematoma are infrequent in the hands of experienced surgeons. However, complications related to mineral metabolism are to be expected.23,24 In the case of the series presented in the article we only had one case of difficult management of hypocalcemia in HPS, this may be explained by the use of indocyanine green that helps to identify the viability of the preserved parathyroid remnant (subtotal parathyroidectomy 7/8).
The case reports presented in this article do not assess patient follow-up but reflect the results in terms of procedural success and adverse events, which are similar to those reported in the international literature.25,26
None.
The authors declare that they have no conflict of interest.

©2023 Parada, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.