Journal of
eISSN: 2373-633X


Case Report Volume 14 Issue 5
General Surgery Department, Hospital Geral of Cuiabá, Brazil
Correspondence: Hellen Cruz Xavier, General Surgery resident in Hospital Geral of Cuiabá, Centro Norte, Cuiabá–MT, Brazil
Received: September 11, 2023 | Published: November 1, 2023
Citation: Xavier HC, Santo GFE, Passos ARO, et al. Minimally invasive techniques in the surgical approach of esophageal leiomyoma: a report case. J Caner Prev Curr Res. 2023;14(5):113-115. DOI: 10.15406/jcpcr.2023.14.00532
Case report: A.L.R, female, complained dysphagia and heartburn with 1-year evolution, not associated with weight loss or other symptoms. EGD (01/03/22): subepithelial lesion in the middle third of the esophagus. Endoscopic ultrasound (01/03/22): hypoechoic, heterogeneous lesion, with precise limits, in the smooth muscle, measuring 3.5x1.2cm. Biopsy (01/06/22): mesenchymal neoplasm. Immunohistochemistry: compatible with benign mesenchymal neoplasm of smooth muscle cells. Chest CT with IV contrast (02/07/23): concentric thickening of the posterior wall in the middle third, extending longitudinally for 4.2 cm. Surgical treatment was chosen due to persistence of symptoms and enlargement of the lesion after 1 year of follow-up. Tumor resection was performed by thoracoscopy with an approach through the right hemithorax. The patient evolved without postoperative complications.
Discussion: Esophageal leiomyoma accounts for 60 –70% benign tumors of the esophagus and less than 1% of all esophageal neoplasms. Up to 50% of patients are asymptomatic and incidentally diagnosed. Symptomatic patients present with dysphagia, heartburn, regurgitation, retrosternal pain. Barium swallow, CT scan with oral contrast and endoscopic ultrasound represent the mainstay of diagnosis. The use of biopsy is controversial and is recommended in cases of diagnostic doubt. Surgery is indicated in symptomatic patients or with tumors > 5cm, or with unclear biological behavior. Thoracoscopy and thoracostomy are standard surgical approaches for upper and middle third tumors. Minimally invasive techniques can be used regardless of the size of the lesion, although lesions > 5cm carry a high risk of conversion to an open surgical. Right surgical approach could create more operating space and avoid affecting the heart and major vessels. Myotomy reapproximation is recommended to prevent loss of peristalsis, bulging of the mucosa and pseudodiverticulum.
Final considerations: Esophageal leiomyomas are rare and, in most cases, do not require surgical intervention. Thoracoscopy approach should be the first choice, whenever is possible, and performed by an experienced surgeon.
Keywords: esophageal leiomyoma, esophagus, thoracotomy, thoracoscopy, benign tumor
EGD, esophagogastroduodenoscopy; EUS, endoscopic ultrasound; GERD, gastroesophageal reflux disease; TC, computed tomography
Esophageal leiomyoma is a rare tumor that originates from connective tissue and is the most common benign tumor of the esophagus corresponding to 2/3 of all benign tumors that affect the organ.1,2 Less than half of patients are symptomatic and are diagnosed incidentally.2 When symptoms are present, they are generally non-specific. In most cases do not require surgical intervention, however surgery (extra mucosal enucleation of the lesion by thoracoscopy or thoracotomy) is the therapeutic mainstay for symptomatic patients and/or for bigger lesions. Tumor enucleation avoids unnecessary esophagectomy and reduces morbidity and mortality, however esophagectomy may be necessary in cases of giant leiomyomas.1,3-5 This article presents a case report of a patient with symptomatic esophageal leiomyoma, measuring 4,5 cm, successful treated surgically through thoracoscopy enucleation.
A.L.R, 37 years old, female, sought health care due to dysphagia and heartburn with 1-year evolution, not associated with weight loss or other symptoms. General physical examination and laboratory tests within normal limits.
Esophagogastroduodenoscopy (EGD) revealed esophagus with preserved caliber and distensibility. Presence of a subepithelial lesion in the middle third, with intact mucosa, measuring approximately 20 mm in its longest axis. Endoscopic ultrasound (EUS): hypoechoic, heterogeneous lesion, with precise limits, in the smooth muscle, measuring 3.5x1.2cm. Two ultrasound-guided punctures were performed for histopathological evaluation.
Biopsy: Spindle cell mesenchymal neoplasm. Immunohistochemistry: Negative for C-KIT (CD 117) and S100, weakly positive for KI-67, positive for desmin, compatible with benign mesenchymal neoplasm of smooth muscle cells.
Chest computed tomography (CT) with IV contrast carried out 1 year after EUS showed concentric thickening of the posterior wall in the middle third, extending longitudinally for 4.2 cm. Surgical treatment was chosen due to persistence of symptoms and enlargement of the lesion after 1 year of follow-up, the procedure was performed by a 30-year experience oncological surgeon. Tumor resection was performed by thoracoscopy with an approach through the right hemithorax. Meticulous dissection was performed all around the esophagus (Figure 1) and the tumor was enucleated without mucosal damage, with approximation of the muscle layer. Surgical piece measuring 4.5x3.2x1.5cm. The esophagus has been checked for leaks.
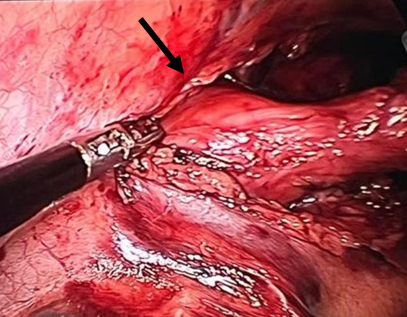
Figure 1 Leiomyoma in the middle third of the esophagus visualized through thoracoscopy, identified by black arrow.
The length of hospital stay was 7 days, during this period the patient remained stable, evolving without complications in the immediate postoperative. After four months of follow-up, she remains free of complications, denying any symptoms of GERD or other symptoms.
Esophageal leiomyoma accounts for 60 –70% benign tumors of the esophagus and less than 1% of all esophageal neoplasms.1,4 They can appear in patients of any age, but they typically occur between the 3rd and 5th decade of life with a predominance in men. The ratio of cases in men and women is approximately 2:1.5,6 Although this pathology is twice as common in men, this report presents a case in female, who are in their 4th decade of life, coinciding with the age range found in the literature.
Esophageal leiomyomas have an extremely low rate of conversion to a malignant lesion.5 They originate from smooth muscles and are intramural, in some cases it may present as a pedunculated polyp. Typically, leiomyomas do not exceed 5cm, however there are reports of giant leiomyomas measuring 20cm.1 Up to 50% of patients are asymptomatic and incidentally diagnosed by chest radiograph and endoscopy. Symptomatic patients present with dysphagia, retrosternal pain, heartburn and regurgitation.1,2 Symptoms are more common in patients with tumors larger than 5cm, revealing that the larger the size of the lesion, the greater the likelihood of symptoms appearing.7
It is known that the size of the lesion is directly related to the presence of symptoms,7 however this does not mean that tumors <5 cm are always asymptomatic. The patient in question began to present symptoms with a tumor measuring just 3,5 cm.
Barium swallow, CT scan with oral contrast and endoscopic ultrasound represent the mainstay of diagnosis.2 All these methods demonstrate the presence of tumor without mucosal injury.1 The use of biopsy for diagnosis is controversial, as it is associated with complications such as: infection, bleeding and perforation, and is recommended when there is diagnostic doubt.1 In the case of the patient in the report EGD was performed for initial investigation and subsequent EUS. Although the use of biopsy for diagnosis is controversial, it was decided to perform it, which revealed a lesion of a benign nature, confirmed through immunohistochemistry. Surgery is indicated in symptomatic patients or with tumors > 5cm, or with unclear biological behavior. Thoracoscopy and thoracostomy are standard surgical approaches for upper and middle third tumors.2,4 Despite thoracoscopic approach could decrease incision size, postoperative trauma, hospital stay duration, and postoperative pain, it cannot be performed under some circumstances that may increase surgical difficulty and risk, such as severe thoracic adhesion and some giant leiomyoma.5
Minimally invasive techniques are best suited for enucleation of small lesions, but recent studies indicate that they can be used in larger lesions, although tumors > 5cm carry a high risk of conversion to thoracostomy.4 When thoracoscopy is the chosen technique, ideally the procedure should be performed with the patient in the prone position. Prone thoracoscopy allows for optimal visualization of the surgical field, better ergonomics and better pre-operative oxygenation.2 Right surgical approach for lesions in upper/middle third esophagus could create more operating space and avoid affecting the heart and major vessels.4,5
Tumor enucleation should be performed without opening the mucosa with blunt dissection between the esophageal muscle fibers. During the procedure, a suture thread can be passed through the tumor to lift and tract the lesion in order to find the proper plane between the tumor, muscularis propria, and underlying submucosa (Figure 2).1,4
For the patient in this report, a minimally invasive procedure was chosen, due to the benefits of this technique, take into account the tumor size and the surgeon’s extensive experience. Prone thoracoscopy was performed and as the lesion was located in the middle third, a right surgical approach was chosen. Laparoscopy trans-hiatal enucleation is indicated in patients with tumors located up to 5cm from the esophagogastric junction and has the advantage of being able to perform crural repair and fundoplication in patients with Gastroesophageal reflux disease (GERD).2
Surgeon experience, tumor size, and irregular shape are risk factors for mucosal perforation and fistula.7 Myotomy reapproximation is recommended to prevent loss of peristalsis, bulging of the mucosa, and pseudodiverticulum. The approximation of the muscular layer can preserve propulsive activity, esophageal clearance and thus reducing the incidence of surgical procedures for GERD.2 Aiming to prevent post-operative complications, the muscular layer was reapproximated, as well as preserving the integrity of the mucosa.
The surgeon's experience is an important determinant of the success of surgery using minimally invasive techniques, especially in the case of larger leiomyomas.4 Recurrence after leiomyoma enucleation is rare, requiring no oncological follow-up, although monitoring is necessary for the appearance of late complications from surgery such as GERD, esophageal diverticulum.4 At the time of this report, the patient is in the fourth month of follow-up and so far, has not had any complications from the procedure. Outpatient follow-up is necessary in the coming months for early identification of possible late postoperative complications.
Esophageal leiomyoma is a rare condition, which in most cases is asymptomatic and is discovered incidentally. When the tumor became symptomatic or bigger than 5 cm requires surgical treatment. Both thoracotomy and thoracoscopy can be used for tumor enucleation, however thoracoscopy approach should be the first choice, whenever possible, and performed by an experienced surgeon.
None.
Authors declare that there are no conflicts of interest in the preparation of this article.

©2023 Xavier, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.