Journal of
eISSN: 2574-9943


Research Article Volume 7 Issue 2
1Dental Surgeon – University Center of Patos de Minas (UNIPAM)
2Dental Surgeon – School of Dentistry of Araçatuba (UNESP), Master in Restorative Dentistry (Dental Sciences–UNESP), Specialist in Orofacial Harmonization (THOPPI Institute)
3Dental Surgeon – Graduated in Dentistry from Universidade Vale do Rio Verde in Três Corações; Specialist in Orofacial Harmonization (CFO)
Correspondence: Emanuelle Teixeira Carrera, Dental Surgeon – School of Dentistry of Araçatuba (UNESP); Master in Restorative Dentistry (Dental Sciences – UNESP), Specialist in Orofacial Harmonization (THOPPI Institute), Tel (16) 98233-7052
Received: June 01, 2023 | Published: June 19, 2023
Citation: Guimarães YKS, Carrera ET,Vieira EAC, et al. Comparative study between subjective facial analysis and cephalometric analysis of soft tissues in the diagnosis of lip repositioning resulting from the perfect nose® technique. J Dermat Cosmetol. 2023;7(2):66-69. DOI: 10.15406/jdc.2023.07.00237
The face is arguably the most important factor in a person's physical appearance, including the smile. In facial aesthetics, the initial objective is to determine the facial type, in order to promote balance and harmony between the hard tissues (teeth and bones) and soft tissues that make up the face. the lateral teleradiographs and the tracings on the teleradiographs performed, the so-called cephalometric analysis, are the most used to study the contour, the relationship between the hard tissues and the soft tissues, and thus, determine the best treatment. Currently, for the aesthetic improvement of the nose, improving its dimensions and proportions, we have the Perfect Nose® technique, a registered, promising and exclusive technique, which, in addition to improving the aesthetics of the nose, can also promote functional improvement. Thus, the objective of this work was to subjectively evaluate, through a comparative study between Subjective Facial Analysis (by means of photography) and Cephalometric Analysis of Soft Tissues (ACTM), the lip repositioning resulting from the Perfect Nose® technique.
Keywords: face, aesthetics, harmony
The face is undoubtedly the most important factor in a person's physical appearance, including the smile.1 In facial aesthetics, the initial objective is to determine the facial type, in order to promote balance and harmony between the hard tissues (teeth and bones) and the soft tissues that make up the face.2,3
With the aim of evaluating and defining a harmonious facial profile, lateral teleradiographs and tracings on the teleradiographs performed, the so-called cephalometric analysis, are the most used to study the contour, relationship between hard tissues and soft tissues, and thus, determine the best treatment.4,5
Aiming at orofacial harmony, several authors stood out with their studies of teleradiographs and cephalometric analysis methods, with the aim of determining facial types. Edward H. Angle (1900) determined the skeletal pattern of the face, based on the vertical imbalance associated with malocclusions in Class I, called a straight profile, Class II, a convex profile due to the mandible being retruse, and Class III, a concave profile because of the protruding mandible. In this classification, it is more common to find patients with Class II facial type, which is also described in the literature as Long face pattern or Hyperdivergent type.4,6
Bimler in 1957, using the angular measurement method to describe the variations between facial types and they were called mesoprosopic or mesocephalic facial type, angle variation between 15° and 30°, harmonious and well-balanced face and class I malocclusions. The other facial type was leptoprosopic or dolichocephalic, with an angle of 30° and 45°, characterized by a long face and convex bone profile. While in the dolicoprosopic or brachycephalic facial type, angle between 0° and 15°, characterizing a short face and concave bone profile.7
Another cephalometric analysis used to classify the facial pattern is that of Ricketts (1982), in which the author determines the coefficient of the amount of vertical growth of the face (VERT), classifying the facial types into dolichofacial, vertical growth tendency, mesofacial, balanced or brachyfacial growth, horizontal facial growth tendency.3
Thus, it is noted how important the classification of the type of facial pattern is during the diagnosis, in order to carry out a good planning and consequently to obtain a good result, since the concern includes the correction of hard tissues, teeth and bones , and the positioning of the soft tissues on the face, as well as the nose, lips and chin.3,8 And in the aesthetic, as well as functional perception of the profile, a very common complaint is the nose, which is an extremely important organ in facial harmony and balance, mainly because it occupies a central position on the face.9
Cephalometry is a radiographic technique from which data are obtained regarding craniofacial development, type of occlusion, facial typology, among others. Face analysis, another fundamental diagnostic tool, can be performed directly or indirectly. Direct or three-dimensional analysis, through clinical examination, promotes a more satisfactory assessment of orofacial structures when compared to the indirect form characterized by two-dimensional analysis performed through cephalometry or photographs.10
Both have as their main objectives the evaluation of facial aesthetic, facial orthopedic, orthodontic and surgical diagnosis, in addition to contributing to treatment planning in both the initial and intermediate stages. considered an important tool to establish the diagnosis, as long as they are standardized and of good quality.10
The Perfect Nose® technique was performed with asepsis of the face and nostrils, with alcoholic chlorhexidine solution and mouthwash with 2% chlorhexidine, then bilateral local anesthesia of the infraorbital nerve and infiltrative anesthesia in the region of the nasal spine, columella, tip of the nose, nasal dorsum and nasal ala. The incision was made with an 11 blade, 1 cm beside the columella, in each nostril, for nasolabial disconnection. Then, an infracartilaginous incision was made in each nostril, detaching the entire incised area, and access to the nasal dorsum, with care and caution with the cartilage.
Afterwards, the nasal tip was sutured using a 2-0 70 cm straight blue nylon thread, entering and exiting the incised nostril region. It was repeated in each nostril with the entry and exit of the thread, to hold the nasal tip, according to the anatomy of the nose. For eversion of the columella, the suture was made using blue nylon thread 3-0 70 cm, curve 3/8.
This step must be repeated according to the columella with the anatomy of the nose, always repeating on each side of the nostril. It ends with the external suture of the incisions made in both nostrils. Then, it is extremely important to wash well and irrigate with sterile saline solution and ozone foam.
Currently, for the aesthetic improvement of the nose, improving its dimensions and proportions, we have the Perfect Nose®11 technique, a registered, promising and safe technique, which, in addition to improving the aesthetics of the nose, can also promote functional improvement.
Thus, the objective of this work was to subjectively evaluate, through a comparative study between Subjective Facial Analysis (by means of photography) and Cephalometric Analysis of Soft Tissues (ACTM), the lip repositioning resulting from the Perfect Nose® technique.
The patient complained about the facial profile. And after going through a careful anamnesis and clinical evaluation by the team's professionals and verifying the indication of the Perfect Nose® procedure, which is an exclusive procedure and registered by the THOPPI Institute, which is a minimally invasive procedure, performed with non-absorbable threads, which provides aesthetic and functional balance of the facial profile, the patient was informed in detail about the procedure, expectations, and essential care in the postoperative period and signed the Free and Informed Consent Form.
For the study, frontal and lateral position photographs (profile), profile teleradiography, both before and after the procedure were required.
To standardize the study, the photographs of the before and after procedure were taken by the same professional and were standardized. And the same occurred for lateral teleradiography, which was performed in the same radiological center, using the same software and by the same professional, in both situations.
Thus, a lateral teleradiography of the patient was requested before the procedure, with USP, Bimler and Ricketts cephalometric analysis, cephalometric tracings and the ACTM tracing. And photos were taken before the procedure.
The minimally invasive technique, Perfect Nose®, was then performed and the patient was discharged after 45 days and then, a new lateral teleradiography was requested, along with USP, Bimler and Ricketts cephalometric analyses, cephalometric tracings and ACTM. As well as, new photographs were taken, following the same initial pattern for analyses.
The patient was classified according to facial type through subjective facial analysis, using front and side photographs, according to the facial pattern.12 (Figures 1 & Figure 2).
The lateral teleradiography was traced using the ACTM12, which evaluates the lower third of the face, verifying the relationship between the maxilla and the mandible, using the True Vertical Line as a reference. Cephalometric tracings were performed using the contracted radiology company's software. The magnitudes measured by the ACTM were obtained by the linear distance between each of the points up to a projection of the True Vertical Line (LVV) passing through the subnasal point (Figure 3).
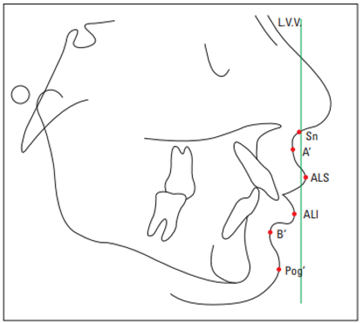
Figure 3 Cephalometric landmarks used in ACTM. Source: Feres et al.,12
To perform the tracing, it is necessary to identify the following soft tissue cephalometric points: Sn (Subnasium), Point A', ALS (upper lip), ALI (lower lip), Point B' and Pog' (pogonion). The nasolabial angle was also evaluated.
After 60 days of the procedure, new photographs were taken (Figures 4 & Figures 5) and new lateral teleradiography with the tracings were requested and the same analyzes mentioned above were performed.
For the Subjective Facial Analysis, photographs of the patient in the frontal and lateral position, before and after the procedure, were evaluated, classifying the patient as class II, division 1 of Angle, dolichocephalic according to Ricketts and leptoprosopic according to Bimler.
For Cephalometric Analysis of Soft Tissues (ACTM), tracings were performed on lateral teleradiography, both before and after the procedure (Figures 6 & Figure 7).
The magnitudes measured by the ACTM were obtained by the linear distance (in centimeters) between each of the points up to a projection of the True Vertical Line (LVV) and the following data were obtained, shown in Table 1.
Greatness |
Linear Distance BEFORE |
Linear Distance AFTER |
ALS |
0.8 |
0.9 |
THERE |
1.0 |
1.2 |
Pog' |
2.6 |
1.8 |
Table 1 Quantities measured by ACTM before and after the procedure
The nasolabial angle (NLA) at baseline and after the procedure were measured on lateral teleradiography, being 85° and 113°, respectively.
The quest for self-esteem through facial aesthetics is increasingly present in the daily lives of the world's population.
The procedures are carried out in order to establish functional, psychological and aesthetic aspects with the obligation and understanding of the normal, always obeying the specific anatomy of each individual as well as the structural variations that compose it. The best treatment is one that respects and values the individual as a whole and offers different options to achieve the expected result. In addition, the individuality of the patient must be taken into account when planning the treatment, as it has been shown that individuals who are supposed to have the same facial characteristics, because they are of the same race, have peculiarities in their facial patterns due to belonging to different geographic locations.13.
For soft tissue analysis, we chose to use cephalometric analysis (ACTM), as it is a well-known analysis used in various parts of the world. Feres et al.,12 in which through subjective facial analysis and cephalometric analysis. The points and planes necessary for measuring the angles and the distance between the upper lip and the columella and the tip of the nose and cephalometry were demarcated, where we compared the angular dimensions of the structures, developing a tracing of the lateral and frontal radiographs of the craniofacial complex.14
By means of lateral teleradiography, which was performed at the same radiological center, using the same software and by the same professional, in both situations, we were able to analyze the following cephalometric points of the soft tissue profile (ACTM): ALS, ALI and Pog'. A USP, Bimler and Ricketts cephalometric analysis was also requested on the patient's lateral teleradiography, with cephalometric tracings. And photos were taken before and after 30 days of the procedure. With this, the following data were obtained: ALS before the procedure 0.8 and after 0.9. The initial ALI was 1.0 and after that it started to measure 1.2 and finally, the Pog´ point 2.6 at the beginning and 1.8 after, where the magnitudes measured by the ACTM were obtained by the linear distance (in centimeters) between each of the points to a projection of the True Vertical Line (LVV).
These data showed us that class II patients have lips behind the true vertical line, as confirmed in other studies.4,12 And even though these alterations between the cephalometric points of the soft profile have also been found in other studies, confirming our results.4,10,12
The nasolabial angle usually varies between 97 and 110° in females,15,16 and varies according to some authors, this data was evaluated before and after the procedure and we obtained the following results, 85° and 113°, respectively. Showing and confirming, according to the literature, that there was an increase in this angle, justifying the lip repositioning after the Perfect Nose technique®.
It was also possible to note that gender has a great influence on these characteristics, as they differ significantly in terms of facial characteristics, if they belong to different genders.13
Among the options used to attribute the aesthetics of the middle third of the face, the nose, being in the center of the face, is the central landmark and knowing that the proportions and nasal symmetry are directly linked to stipulating patterns, automatically influence lip repositioning.14
the perfect nose®It is a surgical procedure, minimally invasive when compared to a rhinoplasty, practically painless, with low risks when performed by a trained professional. And that provides satisfactory results.11
Thus, even with methodological limitations, as it is a subjective analysis of the soft tissues, as well as a cephalometric analysis and a well-executed technique by the professional, it can be argued that this technique provides the repositioning of the lips, when supported by proportionality in soft tissues, influencing the beauty of the facial profile, as analyzed in other studies.14,17
Facial aesthetics has the initial objective of determining the facial type, in order to promote balance and harmony between the hard tissues (teeth and bones) and the soft tissues that make up the face. With the aim of evaluating and defining a harmonious facial profile, the Cephalometric Analysis of Soft Tissues (ACTM), the tracings were performed in the lateral teleradiography, both before and after the procedure, being the most used techniques to study the contour, relation of the tissues hard on soft tissue. We concluded the comparative study between subjective facial analysis and cephalometric analysis with a positive result and a significant lip repositioning resulting from the Perfect nose® technique. In addition to the satisfactory result, it brought an improvement in the facial profile and a significant increase in the patient's self-esteem.
None.
Authors declare there is no conflict of interest.

©2023 Guimarães, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.