Journal of
eISSN: 2373-4345


Case Series Volume 15 Issue 2
Tegucigalpa Francisco Morazán, Universidad Católica de Honduras, Honduras
Correspondence: Dr. Karen Barahona, Catholic University of Honduras (Tegucigalpa MDC), R2 of the specialty of Periodontics and Implantology
Received: April 01, 2024 | Published: April 17, 2024
Citation: Barahona K, Ávila S, Guifarro JJ. New adjuvant alternative: unilamellar honey membrane to improve healing at the palate graft donor site: a clinical case series. J Dent Health Oral Disord Ther. 2024;15(2):57-59 DOI: 10.15406/jdhodt.2024.15.00614
This prospective, observational study evaluated the efficacy of Biofilm at the palatal connective tissue graft donor site. Carried out at the Catholic University of Honduras, Patients selected according to rigorous criteria followed a treatment plan that included the application of Biofilm three times a day. Using clinical photographs; color, contour, and texture analyzes were performed, along with pain assessment using the visual analogue scale (VAS) on postoperative days 3, 7, 14, and 21. The results revealed a consistent improvement in connective tissue color across all age groups, supported by progressive decrease in VAS scores, indicating a significant reduction in postoperative pain. The analysis of contour changes highlighted the ability of the Biofilm to facilitate healing and maintain the structural integrity of the palate, while the analysis of texture changes showed a positive recovery in the surface appearance of the tissues. Together, these findings suggest that the application of Biofilm contributes not only to the aesthetic improvement of the connective tissue but also to the patient's comfort during recovery. Although the study has limitations, such as the lack of a control group, it provides a valuable basis for future research in optimizing postoperative recovery in patients undergoing palatal connective tissue graft procedures. These preliminary results underscore the need for additional research with a more robust design to validate and extend these findings.
Keywords: unilaminar honey membrane, healing, palate graft, texture, color, pain
CTG, connective tissue grafting; VAS, visual analog scale
Connective tissue grafting (CTG), considered one of the best techniques for the treatment of gingival recession, has presented stable long-term results. However, this technique generates morbidity and discomfort in the palatal region due to the removal of the graft at that site.1–4 Healing of oral mucosal and skin wounds follows a similar four-phase pattern: hemostasis, inflammation, proliferation, and matrix remodeling/maturation.1,5–8 Various adjuvant alternatives have been explored to improve healing in similar procedures. In the 1960s, honey was considered a "worthless but harmless substance." Recently, the use of honey in the treatment of wounds, burns and skin ulcers has experienced resurgence, becoming a focus of research, compared to its previous consideration as an 'alternative'. Honey exerts its effects on wound healing through its antimicrobial properties and alteration of physiological and immunological functions. And it helps speed healing when treating partial thickness burns. The successful use of honey has been reported for a multitude of wounds, including burns, surgical sites, infected surgical wounds, chronic ulcers, malignant wounds, and neonatal wounds, among others.9 These potentially beneficial effects can be attributed to its antioxidant, antibacterial and anti-inflammatory properties. The composition of honey depends on the floral source of pollen used to produce it. In general, honey is a mixture of several different categories of compounds, including polyphenols, ascorbic acid, carotenoids, organic acids, enzymes, and other proteins. All of which contributes to making honey a viable nutritional source of antioxidants.10–13
This prospective, observational study examines the effectiveness of Biofilm at the palate connective tissue graft donor site.
Participant selection: Patients who met the inclusion criteria such as systemically healthy patients, patients over 18 years of age, patients without periodontal disease, and non-smoking patients were selected. Each patient was provided with a treatment plan that included application of the Biofilm three times a day (Figure 1).
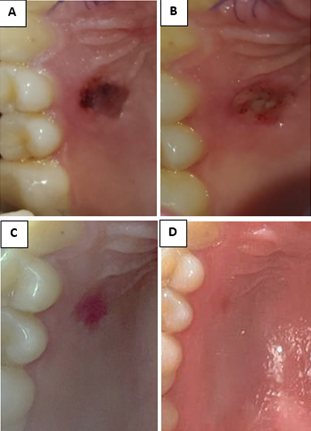
Figure 1 A) Third postoperative day image, B) Seventh postoperative day image, C) Fourteenth postoperative day image, D) Twenty-first postoperative day.
Intervention: Patients were instructed to apply the Biofilm until the 10 ml syringe was exhausted after brushing their teeth and washing the guard provided on the day of surgery.
Follow-up plan: A follow-up plan was established with controls on the third day, seventh day, fourteenth day and twenty-first postoperative day. During these controls, the visual analog scale (VAS) (Figure 2) was used to measure pain, and intraoral photographs were also obtained to evaluate recovery.
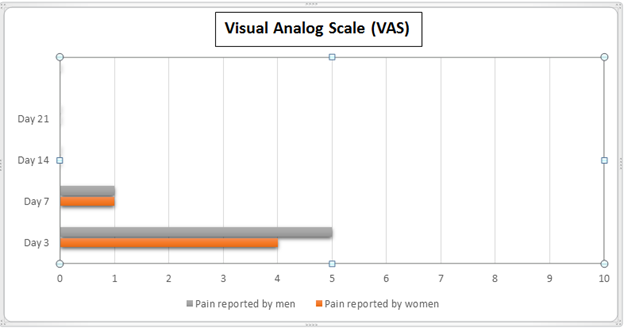
Figure 2 Visual analog scale (VAS).
The chart depicts the pain levels in a group of 11 women and 4 men over several days, using the Visual Analog Scale (VAS). On the third day, women had an average pain level of 4, while men had 5. By the seventh day, the pain decreased to 1 for both groups. On days 14 and 21, both women and men reported an average pain level of 0, indicating an absence of pain.
Scores and analysis: Likert scales were used to analyze changes in color, contour, and texture (Table 1).14–17
|
A |
C |
D |
E |
F |
|
|
Color change analysis |
|||||
|
Age |
Number of patients |
Day 3 |
Day 7 |
Day 14 |
Day 21 |
|
18-28 |
1 |
3 |
3 |
2 |
1 |
|
29-39 |
7 |
3 |
3 |
2 |
1 |
|
40-50 |
6 |
3 |
3 |
2 |
1 |
|
51-60 |
1 |
3 |
3 |
2 |
1 |
|
60 or more |
0 |
Contour change analysis |
|||
|
Age |
Number of patients |
Day 3 |
Day 7 |
Day 14 |
Day 21 |
|
18-28 |
1 |
2 |
2 |
2 |
1 |
|
29-39 |
7 |
2 |
2 |
2 |
1 |
|
40-50 |
6 |
2 |
2 |
2 |
1 |
|
51-60 |
1 |
2 |
2 |
2 |
1 |
|
60 or more |
0 |
Texture change analysis |
|||
|
Age |
Number of patients |
Day 3 |
Day 7 |
Day 14 |
Day 21 |
|
18-28 |
1 |
2 |
2 |
2 |
1 |
|
29-39 |
7 |
2 |
2 |
2 |
1 |
|
40-50 |
6 |
2 |
2 |
2 |
1 |
|
51-60 |
1 |
2 |
2 |
2 |
1 |
|
60 or more |
0 |
Table 1 Likert scale- scores and analysis
A) Color Change Analysis: 1. Exactly similar to the preoperative photograph, 2. Slightly redder than the preoperative photograph, 3. Tissues very red and inflamed, 4. Extremely poor color mismatch. B) Contour Change Analysis: 1. Exactly similar to the preoperative photograph, 2. Some irregularities in the tissues can be detected, 3. Severe depression or extreme elevation of palatal tissues detected. C) Texture Change Analysis: 1. Exactly similar to adjacent tissues, 2. Slightly different from adjacent tissues, 3. Completely different from adjacent tissues.
In this prospective and observational study, the effectiveness of Biofilm applied to the connective tissue graft donor site of the palate was evaluated. The results obtained through the analysis of color, contour, texture and visual analogue scale (VAS) scores provide a comprehensive view of the patients' postoperative response. Regarding color analysis, a consistent improvement is observed in all age groups over time. The application of Biofilm seems to contribute positively to the aesthetics of the connective tissue, reducing inflammation and promoting faster recovery. This finding is supported by the progressive decrease in visual analog scale (VAS) scores, indicating a significant reduction in postoperative pain. The analysis of contour changes shows a structural improvement of the connective tissue, highlighting the ability of the Biofilm to facilitate healing and maintain the integrity of the palatal shape. This result aligns with the decrease in VAS scores, suggesting a relationship between structural improvement and reduction in postoperative pain. Likewise, the analysis of texture changes reveals a positive recovery in the superficial appearance of the palatal tissues. The consistency in textural improvement along with the decrease in VAS scores supports the hypothesis that Biofilm contributes to a complete and harmonious recovery after the procedure.
This study provides promising evidence for the efficacy of Biofilm at the palatal connective tissue graft donor site. The systematic application of Biofilm demonstrated a significant improvement in the color, contour and texture of the connective tissue, supporting the hypothesis that this approach can positively influence postoperative recovery. The progressive reduction in VAS scores indicates an effective decrease in pain levels, suggesting that Biofilm not only improves aesthetics and structure, but also contributes to patient comfort during the critical recovery period. To fully validate these preliminary results and better understand the long-term benefits of Biofilm, additional research with a more robust design, including control groups and extended follow-up, is required. Despite the limitations, this study provides valuable knowledge for optimizing postoperative recovery in patients undergoing palatal connective tissue graft procedures.
I would like to express my sincere gratitude to Dr. Carlos Dumas, the innovator behind the Biofilm unilamellar honey membrane. Their dedication to the research and development of products that positively impact medical practice has been essential to the success of this study. Biofilm proved to be a crucial component in our research on the effectiveness of postoperative recovery of the connective tissue of the palate. Likewise, we extend our recognition to the Farinter commercial house for its generous contribution in providing us with the necessary product to carry out this thesis. Their support has enabled a comprehensive study to be carried out and has enriched our understanding of the clinical applications of Biofilm. We also thank the postgraduate dentistry faculty for giving us the opportunity to carry out this study in their facilities. Their support and collaboration have been invaluable, providing a conducive environment for research and the advancement of knowledge in the field of dentistry.
The authors declare that there are no conflicts of interest.

©2024 Barahona, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.