Journal of
eISSN: 2373-4426


Research Article Volume 14 Issue 1
1Department of Midwifery, College of Health Sciences, Salale University, Ethiopia
2Department of Medicine, College of Health Sciences, Salale University, Ethiopia
Correspondence: Befekadu Tesfaye Oyato, Department of Midwifery, College of Health Sciences, Salale University, Fitche, Ethiopia, Tel +251984779046
Received: January 18, 2024 | Published: February 12, 2024
Citation: Oyato BT, Gutema BG, Feyisa M. Effective breast feeding techniques and associated factors among lactating mothers: a community-based crosssectional study in Dugda district, central Ethiopia. J Pediatr Neonatal Care. 2024;14(1):33-39. DOI: 10.15406/jpnc.2024.14.00538
Background: Breastfeeding technique is defined as the positioning of the mother and baby, the baby's attachment to the breast, and suckling during nursing, all of which are crucial for successful breastfeeding. Appropriate and longer breastfeeding practices have numerous benefits for both mothers and babies. Moreover, ineffective breastfeeding techniques are a cause of death for thousands of newborns every year. In Ethiopia, the practice of effective breastfeeding techniques remained low. Therefore, this study aimed to assess the practice of effective breastfeeding techniques and associated factors among breastfeeding mother-infant pairs in Dugda district, Central Ethiopia, 2023.
Methods: A community-based cross-sectional study was conducted from June 20 to August 20, 2023, in Dugda district on a total of 620 breastfeeding mother-infant pairs who were selected using a multistage sampling technique. Ethical clearance and approval were secured from the Ethical Review Board of Salale University with reference number SLU-IRB/53/23. The WHO's breastfeeding observational checklist and a face-to-face interview were used to collect the data. Bi-variable and multivariable binary logistic regression analyses were employed. An adjusted odds ratio coupled with a 95% CI was used to determine a significant association. Bi-variable and multivariable binary logistic regression analyses were employed. An adjusted odds ratio coupled with a 95% CI was used to determine a significant association.
Results: The prevalence of effective breastfeeding techniques in this study was 43.4% (95% CI: 39.1%, 47.4%). Having antenatal care follow-up (AOR: 2.24; 95% CI: 1.21, 4.14), having prior information about breast feeding techniques (AOR: 5.78; 95% CI: 3.95, 8.46), being multipara (AOR: 2.21; 95% CI: 1.47, 3.33), and having educational levels of primary education (AOR: 2.42; 95% CI: 1.44, 4.06) and secondary education and above (AOR: 2.85; 95% CI: 1.73, 4.69) were significantly associated with effective breastfeeding techniques.
Conclusion: The prevalence of effective breastfeeding techniques in the study area was relatively low. Therefore, empowering women in education, promoting utilisation of ANC follow-up and disseminating information about breastfeeding techniques could be the key implication for effective breastfeeding techniques. Special emphasis should be given to primipara mothers because they are new for nursing their infants.
Keywords: effective breastfeeding technique, lactating mothers, cross-sectional study, Dugda district, Ethiopia
AOR, adjusted odds ratio; ANC, antenatal care; BFT, breastfeeding technique; CI, confidence interval; COR, crude odds ratio; C/S, ceasarian section; EBFT, effective breast feeding technique; EDHS, Ethiopian demographic health survey; PNC, Postnatal Care; SVD, spontaneous vaginal delivery
Breastfeeding is the process of a mother providing her infant with breast milk, either directly from the breast or by expressing breast milk and delivering it to the child in a bottle.1 Breastfeeding technique (BFT) is defined as the positioning of the mothers and babies, the baby's attachment to the breast, and suckling during nursing, all of which are crucial for successful breastfeeding. Appropriate and longer breastfeeding practices had numerous importance for both mothers and babies, such as reduction of overweight, type 2, diabetes, ear infections, asthma, lower respiratory infections, diarrhea and vomiting, eczema, childhood leukemia, and sudden infant death syndrome.2 In addition to helping them with birth spacing, it protects breastfeeding mothers from ovarian and breast cancer.3
Globally, above half a million children and hundred thousands of women die each year as a result of ineffective breastfeeding which could be prohibited by applying appropriate breastfeeding techniques.4 Children's deaths during the first year of life, which account for more than two-thirds of all deaths worldwide, are frequently attributed to improper feeding methods.5 About, 56.8% of children whose mothers did not breastfeed them well suffered from diarrhea, and 62.7% of them developed acute respiratory infections.6
Ineffective breastfeeding technique significantly affects newborn growth and development and it is a cause of death for thousands of newborns every year.7 Nipple cracking, breast engorgement, mastitis, breast abscess in the mother, and poor infant growth and development are the results of ineffective breastfeeding techniques, such as incorrect positioning, attachment, and sucking.8
The practice of effective BFT varies across different settings. For instance, in West Denmark 52%,9 Libya 48%,10 South-East Nigeria 49%,11 South-Ari district, Southern Ethiopia 36.5%,8 Harar city, Eastern Ethiopia 43.4%,12 Gondar town, North Ethiopia 48%.13
Parity, young maternal age, lack of formal education, breast problems, maternal occupation, antenatal care (ANC) and postnatal care (PNC) counseling on breastfeeding, and infants factors like the current age of the infant, birth weight, and health conditions are some of the factors associated with effective BFT.8,12,13
Several methods have been used to solve the issue, but in the last ten years, there hasn't been enough progress.14 In accordance with the recommendations for the Integrated Management of Neonates and Childhood Illness (IMNCI), the WHO and the baby-friendly hospital initiative have created effective BFT counseling, teaching, and demonstrations for mothers in all maternity care services and all mothers of children who are ill.15 Ethiopia has also recently incorporated Ineffective breastfeeding techniques as a diagnostic indicator of severe acute malnutrition for infants under six months in the 2019 Ethiopian national guidelines for the management of acute malnutrition.16
Studies on breastfeeding techniques have been done in Ethiopia, and the majority of them have found a gap in breastfeeding. Additionally, the majority of the studies were carried out among mothers who sought out institution-based health services, meaning that these women were significantly more knowledgeable about healthy practices.8,12,13 Generally, effective breastfeeding has numerous importance for a baby’s growth and development, and maternal health. However, the breastfeeding technique lacks concern and because of this, postpartum mothers and children are exposed to morbidity and mortality. From the authors level of literature review, there was no data on effective BFT and factors affecting it in the study area. Therefore, this study aimed to assess effective breastfeeding techniques and associated factors among lactating mothers in Dugda district, Central Ethiopia, 2023.
Study setting and period
Dugda district is situated in the East Shoa Zone of the Oromia regional state, which is about 118 kilometers away from the capital city of Ethiopia, Addis Ababa. There are 34 rural and 2 urban kebeles in the district. The district is bordered by Hora-Dambal on the southeast, Adami Tullu and Jido Kombolcha on the south, Sododachi district on the northwest, and Bora district on the north. The administrative center of the Dugda district is Meki Town. The district had an estimated population of 15, 2719 in 2022—81,763 men and 70,956 women—according to the report from the Dugda district Health Office. The district was home to 37,131 women of reproductive age, of whom 5830 were nursing babies and 8079 were pregnant. Seventeen private clinics, thirty-one health posts, eleven health centers, and one primary hospital served the district. The study was carried out from July 20, 2023, to August 20, 2023.
Study design
A community-based cross-sectional study was employed.
Study participants and eligibility criteria
All lactating mothers in Dugda district were the source population for this study. The study population included all lactating mothers with children under six months old who lived in the selected kebeles of the Dugda district. Mothers whose infants were born with cleft lips or palates and whose illnesses prevented them from nursing were excluded from the study.
Sample size determination
The actual sample size for the study was determined considering the following assumptions: the level of confidence was taken to be 95% with α=0.05 value (which yields Z α/2=1.96 on the standard normal distribution curve), a 5% margin of error (d=0.05), and a proportion of lactating mothers with an effective BFT of 42.9% from a study conducted in Gidan district, North-East Ethiopia.17 Based on this assumption, the actual sample size for the study was computed using single population proportion formula as indicated below.
....(1)
After applying a design effect of 1.5, the sample size became 564. Taking into account a 10% non-respondent rate, the final sample size for this study was 620.
Sampling technique and procedure
A multistage sampling technique stratified according to urban and rural kebeles was employed in the study. Thirty percent of the total kebeles (10 rural kebeles and 1 urban kebele) out of the 34 rural and 2 urban kebeles found in the district were selected using a simple random sampling technique. There were 1320 lactating mothers who had infants younger than 6 months in selected kebeles. Health extension workers' (HEWs) registration books at each selected Kebele contained a list of nursing moms and their infants under six months old. This list served as a sample frame. Afterwards, taking into account the number of lactating mothers in each chosen kebele, the sample size was adjusted proportionately. The participants were selected at random from each kebele using simple random sampling, which uses a computer-generated number.
Operational and term definition
Breastfeeding technique: The composite of positioning, attachment, and suckling while breastfeeding.13
Positioning: The manner a woman holds her child or their physical alignment. A baby should be positioned according to certain guidelines: their body should be straight and slightly extended; their body should be close to their mother's; their entire body should be supported; and they should be facing the mother's breast.17
Attachment: The manner in which a newborn takes the breast into his mouth and the quantity of breast tissue and areola located in the mouth. A healthy baby attachment meets the following requirements: The infant has a wider mouth, its lower lip turned outward, more areola visible above the top lip, and his chin touching or nearly touching the breast.17
Suckling: The action through which a baby takes breast milk from the mother. Standards for rating successful nursing: sucks slowly, deeply, and occasionally pauses while sucking.13
Effective breastfeeding technique (BFT): A BFT is considered effective if the combined score of the three composite variables—two from positioning, three from attachment, and two from suckling—is greater than or equal to seven. If the score is less than seven, the BFT is considered ineffective.13,17
Family support: Pertains to the assistance that women receive from their relatives, specifically from the husband, the mother-in-law, the grandmother, and other family members regarding their breastfeeding practices.18
Breast problems: Breast problems such as: engorgement, which is characterized by a painful, swollen breast and poor milk supply; crackle, which is a break in the skin; an inverted nipple is one that curves inside rather than out; a sore nipple is one that hurts in the nipple and areola during feeding.
Data collection tools
The data were gathered through the use of the WHO’s breastfeeding observational checklist19 and a face-to-face structured interviewer-administered questionnaire which was adapted and modified from the previous studies.13,17 An expert in language translation translated the English-prepared questionnaires into Afaan Oromo, the local tongue, and then back to English to maintain consistency.
The appropriate positioning, attachment to the breast, and suckling were assessed during breastfeeding using the observational checklist. Information on the clients' socio-demographics, obstetrics and health services, and maternal and newborn health was obtained through questionnaire-based interviews. Eight BSC midwives (data collectors) and two BSc nurses (supervisors) who had previously coordinated and collected data for research projects were enlisted for the data collection.
Data quality assurance
A pretest study was conducted in the Bora District with approximately 5% of the total estimated sample size to confirm the accuracy of the data. For one day, the supervisors and data collectors received orientation regarding the goals of the study and the protocol for gathering data. To reduce interobserver variability, the data collectors were oriented with a focus on how to score the observational checklist. To further reduce interobserver variability, the study employed data collectors with comparable experience and educational backgrounds.
Using an observational checklist, the data collectors first assessed the nursing techniques while a mother fed her child. The mother was then questioned for the remaining portion of the questionnaire. The mothers were instructed to demonstrate how they routinely breastfed their child and that they wouldn’t be judged by their way of doing it. The data collectors observed breastfeeding for a minimum of five minutes, documenting the mother's positioning, attachment, and suckling in accordance with the WHO breastfeeding observational checklist. The observations took place in a private, at-home setting, with the mother.
The investigators reviewed the data on daily during the data collection process to ensure it was accurate, consistent, and complete. If necessary, they promptly made corrections.
Data processing and analysis
The gathered data was coded once its accuracy and consistency were confirmed. The data was entered into Epi Data version 4.6 and exported to SPSS version 26 for analysis. Descriptive statistics, like frequency and percentage, were computed to provide context for the study population in relation to pertinent variables. Positioning, attachment, and sucking were combined to create a single outcome variable for BFT. The results were then divided into two categories: effective and ineffective breast feeding techniques (coded 1 for effective techniques and 0 for ineffective techniques).
To see the relative effect of independent variables on the dependent variable, a binary logistic regression analysis was carried out. Variables with a p value of <0.25 in bi-variable regression were taken into account in the multivariable logistic regression model. The standard ENTER method was used to obtain the final model in the multivariable logistic regression analysis. The adjusted odds ratio (AOR) was used to interpret the strength of the association at 95% CL with a p value of <0.05. Using the Hosmer-Lemeshow good-fit test, the model's fitness was evaluated. Tables, text, frequency, and figures were used to present the outcome in the end.
Ethical consideration
Ethical clearance and approval were secured from the Ethical Review Board of Salale University with reference number SLU-IRB/53/23. Once the Dugda district health office reviewed the letter of support from Salale University College of Health Sciences, they granted permission to conduct the study. Written informed consent to participate in this study was obtained from each study participant after explaining the purpose, procedure, benefits, duration, and any possible risks of the study using the local language. The participant's right to discontinue or leave the study was also secured. The Declaration of Helsinki's guiding principles were followed in the conduct of this study. The entire information collected from the study participants was handled confidentially by omitting their identifiers.
Socio-demographic characteristics of the participants
A total of 608 breastfeeding moms participated in this study, resulting in a 98% response rate. The mean age of participants was 26.39 years (SD±4.451). Approximately 36 percent of the participants were in the 26–30 age range. The infants were between 0 and 6 months old. Of the participants, the proportion of Orthodox and Protestant religious followers was 362 (59.5%) and 96 (15.8%), respectively. Of the participants, 589 (96.9%) were in a union. In terms of education, 167 people (27.5%) had no formal education. The majority of participants—501 (82.4%) and 88 (14.5%)—were housewives and government employees, respectively (Table 1 Socio-demographic characteristics of the study participants in Dugda district, Central Ethiopia, 2023 (n = 608)).
|
Variables |
Categories |
Frequency (n) |
Percent (%) |
|
Infant’s age (in months) |
≤1 month |
24 |
4.0% |
|
2-3 months |
250 |
41.1% |
|
|
4-6 months |
334 |
54.9% |
|
|
Mother’s age (in years) |
<20 |
53 |
8.7% |
|
20-25 |
210 |
34.6% |
|
|
26-30 |
219 |
36% |
|
|
>30 |
126 |
20.7% |
|
|
Residence |
Rural |
559 |
91.9% |
|
Urban |
49 |
8.1% |
|
|
Religion |
Orthodox |
362 |
59.5% |
|
Protestant |
96 |
15.8% |
|
|
Muslim |
67 |
11% |
|
|
Waqefata |
47 |
7.7% |
|
|
Othersa |
36 |
6% |
|
|
Mother’s educational status |
No formal education |
167 |
27.5% |
|
Primary education |
197 |
32.4% |
|
|
Secondary and above |
244 |
40.1% |
|
|
Mother’s occupation |
Housewife |
501 |
82.4% |
|
Government employed |
88 |
14.5% |
|
|
Othersb |
19 |
3.1% |
|
|
Marital status
|
Inunion |
589 |
96.9% |
|
Not inuion |
19 |
3.1% |
|
|
Partner’s educational status (n = 589)
|
No formal education |
129 |
21.9% |
|
Primary education |
240 |
40.7% |
|
|
Secondary and above |
220 |
37.4% |
|
|
Partner’s occupation (n = 589)
|
Farmer |
411 |
69.8% |
|
Government employed |
125 |
21.2% |
|
|
Otherc |
53 |
9% |
Table 1 Socio-demographic characteristics of the study participants in Dugda district, Central Ethiopia, 2023 (n = 608)
Note: Othersa: Catholic and Hawariat; Othersb: daily laborer and NGO employees; Othersc: merchant and student.
Obstetric and health service utilization of participants
Of the participants, 516 (84.9%) had an ANC follow-up during their most recent pregnancy, and 412 (67.8%) of the mothers were multipara. Counseling on breastfeeding techniques (BFT) was given to 490 participants (95%) during their ANC visit. The majority of participants (575, or 94.6%) gave birth in a medical facility, while thirty-three, or 5.4%, gave birth at home. A spontaneous vaginal delivery was the mode of delivery for 564 respondents (92.8%). A total of 575 (94.6%) participants had received PNC services, and 571 (99.99%) of them had BFT counseling during their PNC visit.
Of the participants, 42 (6.9%) reported having experienced breast problems. There were 28 cases (66.7%), 9 cases (21.4%), and 5 cases (11.9%) of breast engorgement, inverted nipple, and nipple crack, respectively. Approximately 527 (86.7%) mothers received support from their families to breastfeed. Three hundred seventy-four mothers (61.5%) reported having no prior knowledge of breast-feeding techniques. Concerning infant birth weight, 507 (88.2%) and 43 (7.5%) infants had a birth weight of 2.5–3.9 kg and <2.5kg, respectively (Table 2 Maternal obstetric and infant characteristics of study participants in Dugda distric, Central Ethiopia, 2023 (n = 608)).
|
Variables |
Categories |
Frequency (n) |
Percent (%) |
|
Parity |
Primipara |
196 |
32.2% |
|
Multipara |
412 |
67.8% |
|
|
ANC service during pregnancy |
Yes |
516 |
84.9% |
|
No |
92 |
15.1% |
|
|
BFT counseling during ANC |
Yes |
490 |
95% |
|
No |
26 |
5% |
|
|
Place of delivery |
Health facility |
575 |
94.6% |
|
Home |
33 |
5.4% |
|
|
Mode of delivery |
SVD |
564 |
92.8% |
|
C/S |
34 |
5.6% |
|
|
Assisted delivery |
10 |
1.6% |
|
|
PNC service after delivery |
Yes |
575 |
94.6% |
|
No |
33 |
5.4% |
|
|
BFT counseling during PNC |
Yes |
571 |
99.3% |
|
No |
4 |
0.7% |
|
|
Breast problem
|
Yes |
42 |
6.9% |
|
No |
566 |
93.1 % |
|
|
Previous information about BFT |
Yes |
234 |
38.5 % |
|
No |
374 |
61.5% |
|
|
Infant’s birth weight |
<2.5kg |
43 |
7.5 % |
|
>2.5 – 3.9 kg |
507 |
88.2 % |
|
|
>4.kg |
25 |
4.3 % |
|
|
Family support on BFT |
Yes |
527 |
86.7% |
|
No |
81 |
13.3% |
Table 2 Maternal obstetric and infant characteristics of study participants in Dugda district, Central Ethiopia, 2023 (n = 608)
Note: ANC, antenatal care; BFT, breastfeeding techniques; C/S, ceasarian section; SVD, spontaneous vaginal delivery; PNC, postnatal care.
Status of effective breastfeeding techniques
The proportion of participants who practiced effective breast-feeding techniques was 43.4% (95% CI: 39.1%, 47.4%) (Figure 1 Proportion of effective breastfeeding techniques among study participants in Dugda district, Central Ethiopia, 2023). Taking into account all three elements of effective breastfeeding techniques, 345 (56.7%), 319 (52.5%), and 451 (74.2%) mothers were found to possess good breastfeeding positioning, attachment, and sucking, respectively (Figure 2 Positioning, attachment and suckling of infant during breastfeeding in Dugda district, Central Ethiopia, 2023).
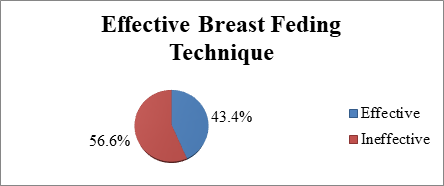
Figure 1 Proportion of effective breastfeeding techniques among study participants in Dugda district, Central Ethiopia, 2023.
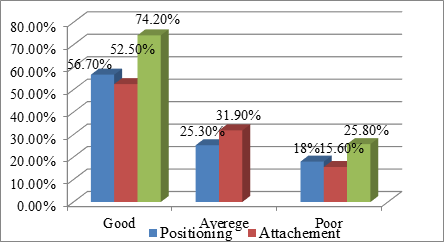
Figure 2 Positioning, attachment and suckling of infant during breastfeeding in Dugda district, Central Ethiopia, 2023.
Factors associated with effective breastfeeding technique
A binary logistic regression model was fitted to determine the variables associated with effective breastfeeding techniques (Table 3 Bivariable and multivariable logistic regression analysis of factors associated with effective breast feeding techniques among study participants in Dugda district, Central Ethiopia, 2023 (n = 608)). Age, mother’s educational status, parity, ANC service received during pregnancy, place of delivery, PNC service received after delivery, breast problem, prior information about BFT, and family support for breastfeeding were all correlated to effective breastfeeding technique in bi-variable logistic regression analysis, with a p-value of less than 0.25. Multivariable logistic regression analysis revealed a significant association, with a p-value of less than 0.05, between the outcome variable and ANC service received during pregnancy, mother’s educational status, parity, and prior information about BFT.
|
Variables |
Categories |
Breast feeding techniques |
COR (95% CI) |
AOR (95% CI) |
|
|
Effective BFT |
Not effective BFT |
||||
|
Mother’s age (in years) |
<20 |
16 (30.2%) |
37 (69.8%) |
1 |
1 |
|
20-25 |
78 (37.1%) |
132 (62.9%) |
1.37 (0.71, 2.62) |
0.94 (0.43, 2.09) |
|
|
26-30 |
114 (52.1%) |
105 (47.9%) |
2.51 (1.32, 4.78) |
1.56 (0.67, 3.65) |
|
|
>30 |
56 (44.4%) |
70 (55.6%) |
1.85 (0.93, 3.66) |
1.36 (0.55, 3.35) |
|
|
Mother’s educational status |
No formal education |
36 (21.6%) |
131 (78.4%) |
1 |
1 |
|
Primary education |
97 (49.2%) |
100 (50.8%) |
3.53 (2.22, 5.61) |
2.42 (1.44, 4.06)* |
|
|
Secondary and above |
131 (53.7%) |
113 (46.3%) |
4.22 (2.70, 6.59) |
2.85 (1.73, 4.69)* |
|
|
Parity
|
Primipara |
62 (31.6%) |
134 (68.4%) |
1 |
1 |
|
Multipara |
202 (49%) |
210 (51%) |
2.08 (1.45, 2.97) |
2.21 (1.47, 3.33)* |
|
|
ANC during pregnancy |
Yes |
246 (47.7%) |
270 (52.3%) |
3.75 (2.18, 6.45) |
2.24 (1.21, 4.14)* |
|
No |
18 (19.6%) |
74 (80.4%) |
1 |
1 |
|
|
Place of delivery |
Health facility |
255 (44.3%) |
320 (55.7%) |
2.12 (0.97, 4.65) |
0.83 (0.30, 2.28) |
|
Home |
9 (27.3%) |
24 (72.7%) |
1 |
1 |
|
|
PNC after delivery |
Yes |
253 (44%) |
322 (56%) |
1.57 (0.75, 3.30) |
0.89 (0.38, 2.09) |
|
No |
11 (33.3%) |
22 (66.7%) |
1 |
1 |
|
|
Breast problem |
Yes |
12 (28.6%) |
30 (71.4%) |
1 |
1 |
|
No |
252 (44.5%) |
314 (55.5%) |
2.01 (1.01, 4.00) |
1.22 (0.5, 2.76) |
|
|
Prior information about BFT |
Yes |
164 (70.1%) |
70 (29.9%) |
6.42 (4.47, 9.22) |
5.78 (3.95, 8.46)* |
|
No |
100 (26.7%) |
274 (73.3%) |
1 |
1 |
|
|
Family support |
Yes |
246 (46.7%) |
281 (53.3%) |
3.06 (1.77, 5.32) |
2.36 (1.11, 5.03) |
|
No |
18 (22.2%) |
63 (77.8%) |
1 |
1 |
|
Table 3 Bivariable and multivariable logistic regression analysis of factors associated with effective breast feeding techniques among study participants in Dugda district, Central Ethiopia, 2023 (n = 608)
Notes: ANC, antenatal care; AOR, adjusted odds ratio; BFT, breastfeeding techniques; CI, confidence interval; COR, crude odds ratio; PNC, postnatal care; 1 = reference; ***statistically significant at p-value < 0.001; ** < 0.01; * < 0.05.
Compared to mothers who had no formal education, the odds of effective BFT were 2.42 (AOR: 2.42; 95% CI: 1.44, 4.06) and 2.85 (AOR: 2.85; 95% CI: 1.73, 4.69) times higher among mothers with primary and secondary education and above, respectively.
According to this study, mothers who had prior information about BFT had 5.78 times higher odds of practicing effective BFT than mothers who had not (AOR: 5.78; 95% CI: 3.95, 8.46). Mothers who received ANC services during their pregnancy were 2.24 times more likely to apply effective BFT than mothers who did not (AOR: 2.24; 95% CI: 1.21, 4.14).
Parity was also significantly associated with effective BFT. The likelihood of multipara mothers practicing effective BFT was 2.21 times higher than that of primipara mothers (AOR: 2.21; 95% CI: 1.47, 3.33) (Table 3 Bivariable and multivariable logistic regression analysis of factors associated with effective breast feeding techniques among study participants in Dugda district, Central Ethiopia, 2023 (n = 608)).
This study aimed to assess effective breastfeeding techniques and associated factors among lactating mothers in Dugda district, Central Ethiopia. Consequently, it was determined that 43.4% (95% CI: 39.1%, 47.4%) of lactating mothers in the Dugda district practiced effective breastfeeding techniques. The results of the study showed a significant association between effective BFT and a mother's educational level, prior BFT knowledge, use of ANC services during pregnancy, and parity.
The prevalence of effective breast-feeding techniques in this study was 43.4% (95% CI: 39.1%, 47.4%). This finding is consistent with research from Gidan district in North-East Ethiopia (42.5%),17 Harar City, Ethiopia (43.4%),12 and Denmark (44%).9 However, this study’s result is higher than research done in Ethiopia's South-Ari district (36.5%).8 Differences in sample size and time intervals between the studies may account for the observed discrepancy. The earlier study involved 415 lactating mothers and was an institution-based study conducted in 2019.
In contrast to research findings from Gondar town, Ethiopia (48%),13 and Libya (48%),10 the prevalence of effective BFT in the current study is lower. A possible explanation could be the different study setting; previous studies were carried out in health facilities that enrolled mothers who come in for immunizations or PNC services. These populations are typically thought to have greater access to breastfeeding counseling and higher health literacy.
The practice of effective BFT was found to be significantly influenced by the respondents' educational status. Compared to moms without any formal education, participants with primary and secondary school education and above had odds of effective BFT that were 2.415 and 2.852 times higher, respectively. This was in accordance with a study done in Harar city,12 Sri Lanka,20 and in western Denmark.9 This is due to the fact that more educated mothers had strong intention and willingness to breastfeed. This factor positively affected the ability of mothers to give more emphasis on instruction, guidance and support from health care providers to have successful breastfeeding technique.
Having ANC follow-up played a pivotal role in application of effective breastfeeding techniques. Mothers who have ANC follow-up were 2.238 times more likely to have effective breastfeeding techniques compared to their counterparts. This is in line 3.w0ith the studies done in Nigeria11 and Wollo, Ethiopia17 This might be explained as ANC follow-up being an ideal entry point for mothers to have services about health and nutritional intervention. So that intervention during pregnancy will have a big role in increasing the mothers' self-confidence, skills, and breastfeeding practices during postnatal periods.
According to the current study, multipara mothers were 2.213 times more likely than primipara mothers to use an effective BFT. This is in line with the findings from studies in South-Ari district, Ethiopia,8 Libiya,10 and Gondar town, North West Ethiopia.13 This could be due to the fact that multiparous mothers might have had frequent BFT counseling and exposure previously, which may enable them to acquire and become proficient in effective breastfeeding techniques.
This study demonstrated that mothers who had previous information about breastfeeding techniques were 5.779 times more likely to practice effective breast-feeding techniques than those who hadn't. This result is similar to findings reported from a study done in East Delhi,21 Harar city, Ethiopia,12 and Southern India.22 The possible justification is that the mother who had previous information will be confident enough to follow the correct techniques, so she will be motivated to know the benefits of exercising the techniques. Information from different sources may enhance their confidence and skill in handling their infant and applying effective breast-feeding techniques.
Using WHO’s breastfeeding observational checklist to assess practice of effective breastfeeding technique was one of the main strengths of the current study. In addition, the study used a large sample size representative of both urban and rural kebeles found in the district.
Despite this, the cross-sectional nature of the study could confirm definitive cause and effect relationship between the variables. Using the registration book as a sampling frame might have been introduced selection bias as new lactating mothers might not get registered.
The overall prevalence of effective breast-feeding technique in the study area was low compared to other studies conducted in Ethiopia. Effective breast-feeding technique was mainly influenced by educational status, parity, ANC follow-up, and prior information of mothers about BFT. To improve breastfeeding techniques among lactating mothers, healthcare providers should prepare community forum in the district, to give health education for the community on effective breast feeding techniques. Health facilities should work in collaboration with community health extension workers to ensure ANC services utilization. Dugda district educational office in-collaboration with other stakeholders needs to empower women in formal education.
The authors are indebted to the Salale University College of health science for the approval of the Ethical clearance. They would also like to express their gratitude to the Dugda district health office and health extension workers for their cooperation through providing necessary informations. Finally, they would like to acknowledge data collectors, and study participants for their cooperation during the study period.
B.T.O. and B.G.G conceived the study, participated in its design and coordination, initiated the research, carried out the statistical analysis, interpreted the results, and wrote the final manuscript, critically reviewing it. M.F. and T.R. participated in the study’s design, guided the statistical analysis, and critically reviewed the manuscript. A.A., H.Z.A., A.G., I.D., H.A, and H.A.D were involved in principal supervision, participated in the study’s design and coordination, edited the manuscript, and critically reviewed the manuscript. B.T.O. has main responsibility for the final content, and makes the decision to publish. The authors have read and approved the final manuscript.
The data that supports the findings of this study are available upon reasonable request from the corresponding author.
Ethics approval and consent to participate
The studies involving human participants were reviewed and approved by Ethical Review Board of Salale University with reference number SLU-IRB/53/23. Written informed consent to participate in this study was obtained from each study participant after explaining the purpose, procedure, benefits, duration, and any possible risks of the study using the local language. The participant's right to discontinue or leave the study was also secured. This study was performed in line with the principles of the Declaration of Helsinki. The entire information collected from the study participants was handled confidentially by omitting their identifiers.
The authors received no funding for this research.
The authors declare that they have no conflicts of interest.

©2024 Oyato, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.