Journal of
eISSN: 2373-4426


Research Article Volume 14 Issue 1
1Department of Midwifery, College of Health Sciences, Salale University, Ethiopia
2Department of Nursing, College of Health Sciences, Salale University, Ethiopia
3Department of Midwifery, Institute of Health Sciences, Jimma University, Ethiopia
Correspondence: Husen Zakir Abasimel, Department of Midwifery, College of Health Sciences, Salale University, Fitche, Ethiopia, Tel +251910331766
Received: January 19, 2024 | Published: February 14, 2024
Citation: Abasimel HZ, Oyato B, Desta AA, et al. Time to death and its predictors among Ethiopian under-five children: cluster-level shared frailty survival analysis using the 2019 Ethiopian mini demographic health survey. J Pediatr Neonatal Care. 2024;14(1):41-50. DOI: 10.15406/jpnc.2024.14.00539
Introduction: Reducing under-five mortality to less than 25 per 1000 live births by 2030 is one of the Sustainable Development Goals introduced in 2016. However, several countries are still falling short of their targets. In Ethiopia, one out of every 19 children dies before reaching the age of five. Thus, this study aims to identify the time to death and its predictors among under-five children in Ethiopia.
Methods: The data were retrieved from the 2019 Ethiopian Mini Demographic and Health Survey data set. Descriptive statistics and survival curves were applied. Shared frailty survival analysis was employed to determine the predictors of under-five mortality. Statistical significance was declared at p-value <0.05.
Result: The under-five mortality rate was found to be 59 deaths per 1000 live births with an estimated mean survival time of 57.6 months (95%CI: 57.38, 57.85). A child born into a family of seven or more had an 85% lowered risk of dying (AHR = 0.15, 95% CI: 0.05, 0.44). The risk of mortality among children born in the birth order of five or above was 3 times higher (AHR = 3.00, 95%CI: 1.70, 5.21) compared to those born in the birth order of one to four. The estimated risk of death among under-five children born less than 24 months interval was 2.68 times higher (AHR=2.68, 95%CI: 1.71, 4.21). Never breastfed was also a significant predictor of under-five child death (AHR = 2.76, 95%CI: 1.46, 5.23).
Conclusion: Birth order, family size, preceding birth interval, and never breastfed history were significant predictors of under-five child mortality. Health policies should focus on keeping the spirit of a continuum of care to improve the health of the child and the health of the family as a whole. Health care providers should intervene in the community to maximize optimal infant and young child feeding practices.
Keywords: time to death, predictors, under-five children, shared frailty, survival analysis
AHR, adjusted hazard rate; ANC, antenatal care; CHR, crude hazard rate; CI, confidence interval; DHS, demographic and health survey; EA, enumeration area; EMDHS, Ethiopian mini demographic and health survey; SDGs, sustainable development goals; U5MR, under-five mortality rate
The under-five mortality rate (U5MR) is a measure of the likelihood that a child will die before turning five and is conveyed as a rate per thousand live births.1 U5MR is a benchmark index of how far a country has advanced in terms of ensuring children's rights, particularly their right to life and protection.2 Infectious diseases, along with preterm birth and intrapartum complications, continue to be a major contributor to preventable under-five deaths worldwide. Furthermore, one-fifth of all deaths in under-five children have been attributed to vaccine-preventable deaths, such as deaths from meningitis, measles, and lower respiratory infections.3
The Sustainable Development Goals (SDGs), which were introduced by the international community in 2016, include the elimination of preventable deaths of children under the age of five as one of their objectives.4 The SDGs target is to reduce under-five mortality to less than 25 per 1000 live births by 2030.4 However, many countries remain off-track to meeting this SDG target.1
The U5MR worldwide was just halved from 2000 to 2020 – falling from 76 to 37 deaths per 1,000 live births. The number of under-five deaths dropped to 5 million in 2020, from 12.5 million in 1990, and from 5.3 million in 2019.1,3,5 Children who are born in Sub-Saharan Africa (SSA) continue to face the world's worst survival rates.1 In 2020, the SSA had an annual mortality rate of 74. This equates to one in every 14 children dying before attaining the age of five, which is 14 times higher than the risk for children in Europe and Northern America and 19 times higher than the risk in Australia and New Zealand.1,6
In 2020, the U5MR in fragile and turmoil nations including Ethiopia was about three times greater than the global average. Those countries accounted for 43 percent of all under-five deaths in 2021.1,7 In 2020, Ethiopia ranked third among nations with the greatest absolute number of under-five deaths.1 One out of every 19 Ethiopian children died before reaching the age of five.8
Place of residence, mothers' education, contraceptive use, breastfeeding status, number of antenatal care visits in pregnancy, child's sex, and vaccination status have all been identified as major predictor variables of under-five child mortality.9–17
A country's future macroeconomic production is negatively impacted by child mortality. It increases healthcare costs, reduces future labor and productivity, and undermines investments in physical and human capital creation.17 Parents who endure child loss also lose a potential source of much-needed economic support in their older age, aside from the emotional trauma they bear for the majority of their lives.18
Ethiopia has made substantial efforts to reduce child mortality under the five-year mark by strengthening healthcare systems, improving equitable access to quality health services, and expanding access to primary healthcare facilities and services.19 Despite this, many children pass away already when they achieve the age of five. As a result, research in this area is critical for determining which health programmes are required for a long-term decrease in under-five child mortality. As a result, millions more children will reach a productive age and contribute to the economy of their country rather than being a financial burden.
Despite the fact that studies have been conducted in Ethiopia, more recent evidence, particularly that accounting for unobserved heterogeneity in risk factors, is required to inform policymakers in order to implement appropriate health intervention strategies to attain the undergoing SDGs. To address this gap, a community-based retrospective analysis was conducted using data from the 2019 Ethiopian Mini Demographic and Health Survey (EMDHS) to examine the time to death and its predictors among Ethiopian under-five children.
Study design and setting
A retrospective cohort study based on the 2019 EMDHS was undertaken by this study. This study was conducted in Ethiopia, which is located on the easternmost point of Africa and bordered to the north by Eritrea, to the east by Djibouti and Somalia, to the west by the Republic of Sudan and South Sudan, and to the south by Kenya.20 With a gross national income per person of US$940 as of 2021, Ethiopia is one of the low-income nations.21 It is the second-most populated country in Africa, with more than 110 million inhabitants.22 The administrative divisions of Ethiopia consist of nine geographic regions and two administrative cities.20 Around 15.5 million of Ethiopia's population, or roughly 18 percent, are under the age of five.22
Data source and populations
The 2019 EMDHS employed a two-stage stratified sampling method to select respondents. 21 strata for sampling were created by dividing each region into urban and rural areas. Each region was stratified into urban and rural areas, yielding 21 sampling strata. The first stage involved the selection of 305 enumeration areas (EAs), of which 93 were urban and 212 were rural. In the second round of selection, 30 households per cluster were randomly selected from the newly constructed household listing with an equal likelihood of systematic selection. Therefore, 9,150 Households (HHs) were selected, and 8,885 women between the ages of 15 and 49 underwent interviews.
All live births that occurred in the five years prior to the survey period across the nation made up the source population. All children under the age of five who were born in the chosen clusters or EAs, five years prior to the survey period were the study populations. As a result, 5,753 children born between 2015 and 2019 were included in this study (Figure 1) Sampling procedure for under-five child mortality from the 2019 Ethiopian Mini-Demographic and Health Survey, 2022). Information on under-five child mortality was taken from the birth history section of the Woman Questionnaire, which was a component of the survey. The data sources were gathered from the standard DHS dataset's under-five children's (KR) file.
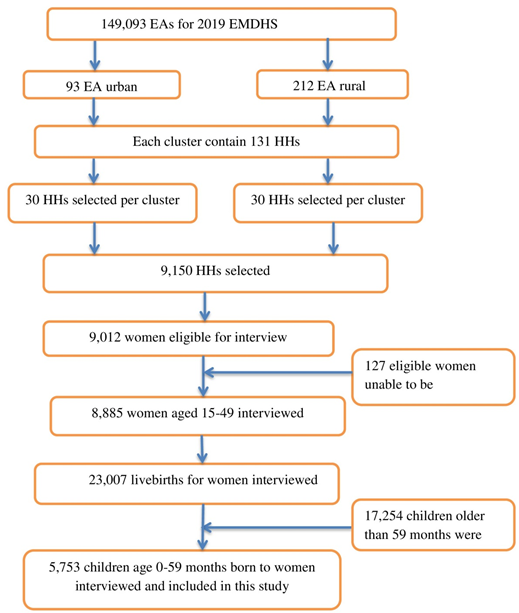
Figure 1 Sampling procedure for under-five child mortality from the 2019 Ethiopian Mini-Demographic and Health Survey, 2022.
Ethical considerations
This study was conducted after obtaining a written permission letter from the Institutional Review Board (IRB) of Demographic and Health Survey (DHS) program data archivists. The dataset is publicly available in requesting a concept note for a proposed project. Consent to participate in the DHS is the responsibility of the institution in charge of the original survey. The information has only been used for this authorized study project, and it will not be shared with any other researchers.
Data abstraction and selection of variables
Dependent variable
The outcome variables is the survival time of a child measured in months from birth until death or the censor of a child before 60 months of age.
Independent variables
The independent variables explored in the study were taken from Mosley and Chen's (1984) determinants of childhood morbidity and mortality framework for developing countries, previous similar studies,9,14,15,23 and available data in the data set. The independent variables in this study ranged from socio-economic factors to variables specific to the mother and the child. The independent variables in this study include mothers’ educational status, place of delivery, marital status, mother’s age at first birth, source of drinking water, type of toilet facility, type of cooking fuel, and floor material of the house (Supplemental Table 1). The variables were also categorized to make it easy for analysis purposes.
|
Variable |
Description |
|
Birth order |
0 = First to Fourth (Reference), 1 = Fifth and above |
|
Preceding birth interval |
0 = 24 and above months (Reference), 1= below 24 months |
|
Religion |
0 = Orthodox (Reference), 1 = Protestant, 2 = Muslim, 3 = Other |
|
Household size |
0 = 1 to 3 (Reference), 1 = 4 to 6, 2 = 7 and above |
|
Maternal education |
0 = No education (Reference), 1 = Primary, 2 = Secondary & above |
|
Marital status |
0 = Married (Reference), 1 = Single |
|
Sex of child |
0 = Female (Reference), 1 = Male |
|
Type of cooking fuel |
0 = Electricity (Reference), 1 = Wood, 2 = Others |
|
Source of drinking water |
0 = Improved (Reference), 1 = Un improved, 2 = Others |
|
Household head |
0 = Female (Reference), 1 = Male |
|
Mother’s age at first birth |
0 = 20-35 years (Reference), 1 = <20 years, 2 = >35 years |
|
Baby checked after birth before discharge |
0 = Yes (Reference), 1 = No, 2 = Don’t know |
|
Main wall material |
0 = Finished (Reference), 1 = Natural, 2 = Rudimentary, 3 = Others |
|
Main roof material |
0 = Finished (Reference), 1 = Natural, 2 = Rudimentary, 3 = Others |
|
Current maternal age |
0 = ≥35 years (Reference), 1 = 25–34 years, 2 = <25 years |
|
Wealth Index |
0 = Rich (Reference), 1 = Poor, 2 = Middle |
|
Breastfed history |
0 = Yes (Reference), 1 = No |
|
Place of delivery |
0 = Health facility (Reference), 1 = Home |
|
Contraceptive use |
0 = Using (Reference), 1 = Not using |
|
ANC utilization |
0 = At least 4 (Reference), 1 = No visit, 2 = 1-3 visits, 3 = Don’t know |
|
Maternal check-up at home |
0 = Yes (Reference), 1 = No |
|
Media access |
0 = Both Tv and radio (Reference), 1 = Either, 2 = Neither Tv nor radio |
|
Mode of delivery |
0 = Vaginal delivery (Reference), 1 = Cesarean-section |
|
Currently pregnant |
0 = No (Reference), 1 = Yes |
|
Place of residence |
0 = Urban (Reference), 1 = Rural |
Supplemental Table 1 Categorization of study variables
Operational definitions
Censored: a child failed to experience the event of interest, which is death.23
Antenatal care utilization: mothers who attended at least four antenatal appointments.24
Data quality control and assurance
The original work's data set was gathered using well-organized, thoroughly-tested standard questionnaires. Face-to-face interviews with women who met the eligibility requirements were used to gather data. To collect the necessary information, the Health Facility Questionnaire, the Household Questionnaire, and the Woman's Questionnaire were all used. The quality of the dataset was maintained by checking its completeness. Aside from that, interviewers were trained, and they used tablet computers to record responses all throughout the interviews, maintaining the integrity of the initial data set.
Prior to statistical analysis, the data were weighted using sampling weight for this study in order to restore the data's representativeness and to obtain a trustworthy estimate and standard error. The study displayed the findings from the weighted analysis. Variance Inflation Factor (VIF) was employed to test for multicollinearity amongst independent variables, and the average VIF value was 1.32 (Supplemental Table 2). Scaled Schoenfeld residuals were also used to assess the proportional hazards (PH) assumption, and a global test value of 0.0680 showed that the assumption was fulfilled. The data was also assessed for potential confounding and interaction factor.
|
Variable |
VIF |
1/VIF (Tolerance) |
|
Birth order |
2.02 |
0.495502 |
|
Mother’s age |
1.62 |
0.617683 |
|
Household size |
1.55 |
0.644949 |
|
Wealth |
1.38 |
0.723144 |
|
Mother’s education |
1.36 |
0.737094 |
|
Religious affiliation |
1.31 |
0.762988 |
|
Electricity access |
1.30 |
0.768825 |
|
Place of delivery |
1.29 |
0.775217 |
|
Roof material |
1.23 |
0.812736 |
|
Mother’s age at first birth |
1.22 |
0.820954 |
|
Contraceptive use |
1.17 |
0.857150 |
|
Region |
1.16 |
0.865136 |
|
Toilet facility |
1.10 |
0.905525 |
|
Preceding birth interval |
1.08 |
0.929992 |
|
Breastfed History |
1.02 |
0.979802 |
|
Mean VIF |
1.32 |
|
Supplemental Table 2 Multicollinearity diagnostics among independent variables
Data management and analysis
STATA version 14 software was used for cleaning, recoding, and analyzing the data. Descriptive statistics were applied using frequencies and percentages. Estimation of survival probability was done by using the Kaplan Meier survival curve and was compared by log-rank test. Bivariable survival analysis was first done for explanatory variables, and those having a p-value ≤0.20 level of significance were considered for the multivariable analysis. Then, backward stepwise variable selection procedure was used to obtain the final model. Finally, multivariable parametric cluster-level shared frailty survival analysis was fitted. Adjusted hazard ratio with its 95% confidence interval was applied, and variables with a p-value < 0.05 in the multivariable analysis were considered predictors of under-five child mortality.
Survival analysis
Survival analysis deals with the analysis of survival statistics, which is applied to estimate the time until an event of interest, such as recovery, relapse, or death.25 The survival times for subjects who left the study early or who finished it without experiencing the event of interest are censored. Each uncensored observation is taken to indicate an event or death.26
Let T denote the random variable for the survival time of a subject. Assume , , denote the probability density function (pdf) of T, and let , be the cumulative distribution function (CDF) of T. The distribution of T is called the survival time distribution. The survival function, S(t), is defined as the probability that a subject survives up to time t:25,26
…………………….(1)
Modeling of parametric survival analysis
A parametric survival model is one in which the survival time is expected to follow a known distribution, which can only be completely described when the parameter's value is known. The Gompertz model is a parametric proportional hazards model. The model can be described similarly to a Cox Proportional Hazards (Cox PH) model, with the exception that the baseline hazard is defined as the risk of a Gompertz distribution with a shape parameter γ.26
If γ > 0 then, the hazard exponentially increases over time. If γ < 0 or negative then the hazard exponentially decreases as time goes on. If γ = 0 then the hazard is constant and reduces to the exponential parametric hazards model.
……………………(2)
Where is the baseline hazard function .
Hence, a parametric model was fitted using Gompertz baseline hazard distributional assumption with a gamma frailty distribution.
Modeling of parametric shared frailty survival analysis
The frailty model is a random-effects model that affects the hazard rate for every person in the same group in an unobserved multiplicative way. This model makes the assumption that groups of subjects have a similar frailty.
The conditional hazard function for the jth subject from the kth cluster in a shared frailty model can be written as αk times hjk(t), where hjk(t) depends on the subject's covariates Xjk. Notice that the frailty αk is subscripted by k, but not by j. This shows that individuals within the same cluster have similar frailties. Children in the same cluster are presummed to share the same nuisance (frailty) component in this shared frailty model.
Hazard conditional on shared frailty (for jth subject in kth cluster) given as.27
……………………(3)
Where , for j=1, 2,. . ., nk and total nk subjects in kth cluster, αk is the cluster level frailty.
The frailties in the model assumed unobservable unit mean and variance θ which is unknown.
Here, αk's reflect variability, and this shows heterogeneity of risks between clusters. According to the model, children from the same clusters are independent, as indicated by the value of 0 frailty. As a result, the range of the random effects' variance is 0 to α. Thus, considerable heterogeneity between clusters is demonstrated by large variance values. Additionally, it demonstrates a stronger association between kids in the same clusters.
Hence, a parametric frailty model was applied in the cluster regarded as random effects frailty for the independent variables using the Gompertz baseline hazard distributional assumption and a gamma frailty distribution model.
Model fitness
Model fitness was checked using Akakian Information Criteria (AIC) and Bayesian Information Criteria (BIC). The lowest AIC and BIC value declare the best fit model. Furthermore, Model assumption fitness was checked using the survival distribution function when all the covariates estimated values were at their mean value.
Socio-demographic characteristics of the study participants
The total numbers of births considered for this study were 5,753 (unweighted). Almost half 2,828 (51.2%) of the study participants were from a household of four to six members with 118 (4.2%) under-five child death. A higher death 75 (11.7%) was recorded among under-five children from a household of one to three. Most 3,537 (64%) of the children utilized water from an improved source, of those 181 (5.1%) children were forced to leave this earth before their fifth birthday. Furthermore, 94 (4.8%) children who utilized water from unimproved sources died before the age of five.
Children from a household led by a male head had a higher under-five death 233 (4.9%) than those whose house head was female 43 (5.7%). Nearly one-third of the children were from a HH who had no toilet facility, of whom 106 (6%) were died before their fifth birth day (Table 1).
Under-five children and maternal obstetric characteristics of the study participants
Almost one-third 1,908 (34.5%) of the children had a birth order of five or more, of whom 115 (6%) lost their lives before their fifth birthday. In addition, 161 (4.45%) children who had a birth order of one to four died. Of the total births, 159 (4.6%) and 117 (5.2%) of under-five deaths have occurred for males and females, respectively. While accounting for 367 (6.64%) of the total children, 110 (30%) never breastfed children died before the age of five. The majority 3,381 (86.1%) of children didn’t get postnatal check-ups within 2 months of birth, of whom 143 (4.23%) children died before the age of five. Moreover, children who were delivered by cesarean section had a higher under-five death 24 (8%) compared to their counterparts 252 (4.82%).
Half 2,842 (51.4%) of the children were delivered at home, of whom 154 (5.42%) died before their fifth birthday. Additionally, 122 (4.54%) children who were delivered at health facilities died before the age of five. Regarding the mother’s age at first birth, 15 (0.27%) children were from mothers of age above 35 years, out of whom 20% died before the age of five years. Another 3,510 (63.5%) children were born to mothers of age below 20 years at first childbirth (Table 1).
|
Covariates |
Category |
Censored N (%) |
Dead N (%) |
Total N (%) |
|
Maternal education |
Secondary and above Primary No education |
591(97) 1858(95) 2802(94.6) |
18(3) 98(5) 160(5.4) |
609(11) 1956(35.4) 2962(53.6) |
|
Current maternal age |
≥35 years 25–34 years <25 years |
1200(93.53) 2829(95.9) 1222(94.36) |
83(6.47) 120(4.1) 73(5.64) |
1283(23.2) 2949(53.36) 1295(23.44) |
|
Main wall material |
Finished Natural Rudimentary Other |
455(96.2) 534(92.2) 4197(95.2) 65(97) |
18(3.8) 45(7.8) 211(4.8) 2(3) |
473(8.56) 579(10.47) 4408(79.75) 67(1.22) |
|
Main roof material |
Finished Natural Rudimentary Other |
3346(95) 1295(94.3) 565(95.9) 45(97.8) |
173(5) 78(5.7) 24(4.1) 1(2.2) |
3519(63.67) 1373(24.84) 589(10.66) 46(0.83) |
|
Wealth Index |
Rich Poor Middle |
1886(96) 2368(94) 996(95.4) |
79(4) 150(6) 48(4.6) |
1965(35.55) 2518(45.56) 1044(18.89) |
|
Type of cooking fuel |
Electricity Wood Other |
261(96.67) 4432(95) 558(94.6) |
9(3.33) 235(5) 32(5.4) |
270(4.9) 4667(84.4) 590(10.7) |
|
Ever breastfed history |
Yes No |
4994(96.78) 257(70) |
166(3.22) 110(30) |
5160(93.36) 367(6.64) |
|
Place of delivery |
Health facility Home |
2563(95.46) 2688(94.58) |
122(4.54) 154(5.42) |
2685(48.6) 2842(51.4) |
|
Current use contraceptive |
Using Not using |
2173(96.5) 3078(94) |
79(3.5) 197(6) |
2252(40.75) 3275(59.25) |
|
ANC utilization |
At least 4 No visit 1-3 visits Don’t know |
1641(97.2) 936(93.2) 1185(96.7) 8(80) |
47(2.8) 68(6.8) 40(3.3) 2(20) |
1688(43) 1004(25.55) 1225(31.2) 10(0.25) |
|
Mother's health checked at home |
Yes No |
400(98.77) 3371(95.7) |
5(1.23) 151(4.3) |
405(10.3) 3522(89.7) |
|
Mother's health checked at facility |
Yes No |
1193(96) 751(96) |
50(4) 31(4) |
1243(61.4) 782(38.6) |
Table 1 Summary of under-five children, maternal obstetrics and socioeconomic-demographic characteristics of study participants in Ethiopia using the recent (2019) demographic and health survey data (5527), 2022
Under-five children’s survival in Ethiopia
A total of 5753 under-five children were followed for a minimum of 1 and a maximum of 59 months with an average follow-up time of 29.2 months. The cumulative probability of survival at the end of the follow-up time was 88.87% (95%CI: 0.8770, 0.8994) with an estimated mean (restricted) survival time of 57.6 months (95%CI: 57.38, 57.85).
Among all under-five children, 339 (5.9%) were dead while the rest 5,414 (94.1%) were censored. The overall incidence rate was found to be 6.3 per 10,000 person month of observation.
Kaplan-Meier survival analysis
The survival probability is very low at an earlier age, particularly before 2 years of age, and starts to settle after the child celebrates his second birthday. As the age increased to 60 months, child deaths significantly decreased (Figure 2 The overall Kaplan-Meier survival estimate among under-five children in Ethiopia using the recent (2019) demographic and health survey data, 2022). Figure 3 shows that compared to children who had previously breastfed, children who had never done so had a greater chance of dying (Figure 3 The Kaplan-Meier survival estimate by ever breastfed history among under-five children in Ethiopia using the recent (2019) demographic and health survey data, 2022).
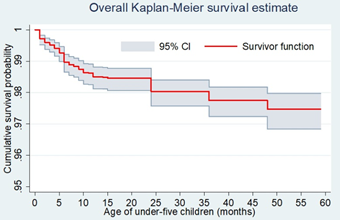
Figure 2 The overall Kaplan-Meier survival estimate among under-five children in Ethiopia using the recent (2019) demographic and health survey data, 2022.
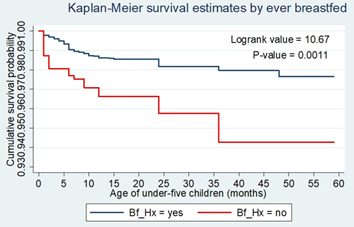
Figure 3 The Kaplan-Meier survival estimate by ever breastfed history among under-five children in Ethiopia using the recent (2019) demographic and health survey data, 2022.
Log-rank test
The log-rank test was used to determine whether there was a statistically significant difference in the survival outcomes of two or more groups of a covariate.
Covariates like ever breastfed history, place of delivery, wealth index, availability of electricity, access to media, route of delivery, and mother’s level of education exhibited a significant difference. Variables including household head, child health checked after delivery, maternal PNC at a facility, water source, type of cooking fuel, and sexes of the child did not experience a significant difference in the survival times of their categories at the 20% level of significance (Table 2).
|
Covariates |
Categories |
Events observed |
Events expected |
Chi-Square |
Df |
Pr>chi-square |
|
Age at first birth |
20-35 years <20 years >35 years |
31 65 2 |
35 63 0 |
22.88 |
2 |
0.0000 |
|
Preceding birth interval |
≥24 months <24 months |
48 39 |
66 21 |
21.66 |
1 |
0.0000 |
|
Current maternal age |
≥35 years 25-34 years <25 years |
37 47 14 |
24 53 21 |
10.89 |
2 |
0.0043 |
|
Baby checked after birth before discharge |
Yes No Don’t know |
8 10 3 |
13 7 1 |
9.98 |
2 |
0.0068 |
|
Main wall material |
Finished Natural Rudimentary Others |
4 17 77 0 |
8 11 78 1 |
8.01 |
3 |
0.0458 |
|
Main roof material |
Finished Natural Rudimentary Others |
52 35 11 0 |
62 24 11 1 |
6.82 |
3 |
0.0780 |
|
Marital status |
Married Single |
90 8 |
92 6 |
1.71 |
1 |
0.1909 |
|
Sex of child |
Female Male |
44 54 |
48 50 |
0.72 |
1 |
0.3965 |
|
Type of cooking fuel |
Electricity Wood Others |
2 84 12 |
5 83 10 |
1.40 |
2 |
0.4959 |
|
Source of drinking water |
Improved Un improved Other |
59 39 0 |
63 34 1 |
1.39 |
2 |
0.4994 |
|
Household head |
Male Female |
84 14 |
84 14 |
0.01 |
1 |
0.9031 |
Table 2 Log-rank test of equality of survival times for covariates among study participants in Ethiopia using the recent (2019) demographic and health survey data (5527), 2022
Model comparison and fitness
The study tried to fit different baseline hazard parametric distributional assumptions. Based on the Akaike Information Criterion (AIC) and the Bayesian Information Criteria (BIC), the Gompertz hazard model with gamma frailty distribution was found the best model to fit the data with a minimum AIC and BIC values of 1017.97 and 1106.94, respectively (Table 3). The model with Inverse-Gaussian distribution had no such significant difference to gamma.
|
Model |
Parameters |
Frailty(theta, p-value) |
-2LogL value (Full) |
AIC value |
BIC value |
|
Cox-PH |
12 |
1.54; 0.000 |
1275.71 |
1299.71 |
1375.54 |
|
Exponential |
14 |
0.57; 0.017 |
1011.78 |
1039.78 |
1128.74 |
|
Weibull |
15 |
0.45; 0.039 |
986.68 |
1016.68 |
1112.00 |
|
Log-normal |
15 |
0.43; 0.046 |
982.17 |
1012.17 |
1107.49 |
|
Log-logistic |
14 |
0.44; 0.042 |
985.94 |
1015.94 |
1111.26 |
|
Gompertz |
15 |
0.41; 0.047 |
979.74 |
1009.74 |
1105.06 |
Table 3 Comparison of different models for time to death and its predictors among under-five children in Ethiopia using the recent (2019) demographic and health survey data (5527), 2022
As shown in Figure 4, the hazard of death among under-five children decreases exponentially as the age of a child increases (Figure 4 Overall Hazard curve at the mean of all covariates among under-five children in Ethiopia using the recent (2019) demographic and health survey data, 2022). This satisfies the Gompertz baseline hazards model assumption that the log (-log) survival estimate is linear with the log of time. Thus, it is evident that the model provided a good fit for the data.
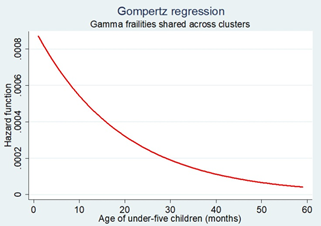
Figure 4 Overall Hazard curve at the mean of all covariates among under-five children in Ethiopia using the recent (2019) demographic and health survey data, 2022.
Factors associated with under-five child death
To identify predictors of under-five child death in Ethiopia, a parametric Gompertz distributional survival model with a cluster level shared gamma frailty distribution was fitted.
In univariate survival analysis variables such as the age of the mother, wealth index, maternal educational level, toilet facility, maternal age at first birth, birth order, preceding birth interval, family size, contraceptive usage, main wall material, and roof material showed statistical significance at the 20% level of significance. All of these factors were therefore taken into account in the multivariable regression model. The final reduced model was then obtained by the study using a stepwise variable removal procedure.
The value of the shape parameter (gamma) in the final Gompertz baseline hazard distribution model was (g = -0.05, 95%CI: -0.07, -0.03). This negative figure shows that as the age of children under the age of five advanced, the risk of death exponentially decreased. The results from the model revealed that preceding birth interval, family size, birth order, breastfed history, and religious affiliation were statistically significant predictors of under-five child mortality (Table 4).
|
Variable |
Categories |
Child status |
CHR(95%CI) |
AHR(95% CI) |
|||
|
Dead |
Censored |
|
|||||
|
Age of mothers |
35 and above |
83 |
1200 |
1 |
1 |
||
|
25 – 34 years |
120 |
2829 |
0.55(0.36, 0.86)** |
0.64(0.39, 1.06) |
|||
|
<25 years |
73 |
1222 |
0.43(0.23, 0.81)** |
0.40(0.14, 1.09) |
|||
|
Breastfed history |
No |
166 |
4994 |
1 |
1 |
||
|
Yes |
110 |
257 |
2.71(1.46, 5.00)** |
2.79(1.46, 5.30)** |
|||
|
Maternal education |
No education |
191 |
2958 |
1 |
1 |
||
|
Primary |
122 |
1701 |
0.76(0.49, 1.19) |
0.88(0.53, 1.49) |
|||
|
Secondary & above |
26 |
755 |
0.24(0.07, 0.80)* |
0.07(0.01, 2.19) |
|||
|
Birth interval |
≥24 months <24 months |
116 93 |
3209 888 |
1 2.47(1.6, 3.82)*** |
1 2.39(1.52, 3.75)*** |
||
|
Family size |
1 to 3 |
75 |
567 |
1 |
1 |
||
|
4 to 6 |
118 |
2710 |
0.72(0.39, 1.33) |
0.53(0.19, 1.50) |
|||
|
7 and above |
83 |
1974 |
0.49(0.25, 0.97)* |
0.12(0.04, 0.36)*** |
|||
|
Religion |
Orthodox |
71 |
1541 |
1 |
1 |
||
|
Protestant |
50 |
1003 |
0.96(0.50, 1.85) |
1.11(0.54, 2.31) |
|||
|
Muslim |
210 |
2764 |
2.04(1.19, 3.51)* |
2.24(1.22, 4.13)* |
|||
|
Other |
8 |
106 |
2.29(0.65, 8.05) |
1.74(0.47, 6.39) |
|||
|
Birth order |
First to four |
161 |
3458 |
1 |
1 |
||
|
Five or more |
115 |
1793 |
1.92(1.28, 2.88)** |
2.78(1.58, 4.88)*** |
|||
|
Constant 0.002(0.0006, 0.007)*** /gamma -0.05(-0.07, -0.03)*** /theta 0.41(P-value=0.047) |
|
||||||
|
P-value |
***<0.001 |
**<0.01 *<0.05 |
|||||
Table 4 Results of bivariable and multivariable parametric Gompertz distribution cluster-level shared frailty survival regression model of under-five children in Ethiopia (5527), 2022
Preceding birth interval was established to be a strong determinant of under-five child fatalities. The estimated risk of death among under-five children born less than 24 months interval was 2.68 times higher (AHR=2.68, 95%CI: 1.71, 4.21) than those born 24 or above months interval. Similarly, the risk of death was 2.76 times higher in children who had never been breastfed than in those who had breastfed at any point in time (AHR=2.76, 95%CI: 1.46, 5.23).
The mortality risk of an under-five child was found to have a negative association with family size. A child born into a family of seven or more had an 85% lowered risk of death relative to those born in a family of at most three members (AHR=0.15, 95%CI: 0.05, 0.44).
Birth order was also a significant predictor of under-five child death. The risk of mortality among children born in the birth order of five or above was 3 times higher compared to those born in the birth order of one to four (AHR = 3.00, 95%CI: 1.70, 5.21). Similar to this, children born to Muslim mothers had a higher risk of dying before five years of age than children whose mothers followed an Orthodox religion (AHR = 2.24, 95% CI: 1.22, 4.13).
This study tried to assess the time to death of an under-five children and its predictors in Ethiopia using the recent 2019 Ethiopian Mini Demographic Health Survey data set, with a cluster-based shared frailty analysis. Hence, it was found that preceding birth interval, household size, birth order, breastfed history, and religious affiliation were significant predictors of mortality in under-five children in Ethiopia.
The study determined a mean survival time of 57.6 months (95%CI: 57.38, 57.85). This is considerably more when compared to Sudan. The median survival time for children under the age of five in Sudan was reported to be 2.3 years (27 months).28 This finding is also higher than what was noted in the Tigray regional state of Ethiopia, where the median survival time for children under the age of five was 26 months.29 This result is also higher than what Argawu's study in Ethiopia found, which was 55.4 months.23 This finding suggests that under-five child survival rates have improved in Ethiopia.
The findings of this study demonstrated a decreasing mortality among children under the age of five with larger family sizes. The results of some prior investigations support this argument. According to a multilevel survival study conducted in Ethiopia, children from families with four to six members and more had a reduced probability of passing away before the age of five than those from families with one to three members.23 A study conducted in rural Ethiopia found that having a larger family size decreased the chance of death among children under the age of five by fifty-six percent.30
On the other hand, a study by Gebretsadik using the 2011 DHS data in Ethiopia found a direct relationship between family size and mortality among children under the age of five.31 The discrepancy could be the result of Gebretsadik’s usage of lesser sample size (2,097). Additionally, this could be the result of the fact that this study and Gebretsadik's study were carried out at different times and using different models. Gebretsadik’s study was carried out only in regions of Ethiopia with substantial fatality rates, applying the Cox proportional hazards model.
The study found that children born in the fifth and higher birth orders had a higher risk of dying before the age of five than those born between the first and the fourth birth orders, which is similar to a study done by Woldeamanuel in Ethiopia.32 Additionally, a study from India reported that higher birth orders significantly influenced under-five child deaths compared to low birth orders.33
This might be the result of higher birth order children being more likely to compete for nutrients and other scarce household resources while also being less likely to get care and attention. The mothers of these children may also neglect to seek the appropriate care from medical facilities because they already have enough children.34 Furthermore, mothers of these children may be more likely to suffer from malnutrition, which makes it harder for the child to obtain enough nutrients from her and increases the risk of infection and malnutrition.
The results showed that children who weren’t breastfed had a significantly greater risk of dying before the age of five. According to a previous study, optimal breastfeeding practices during infancy and early childhood—even partial breastfeeding were protective against mortality.35 A study in Côte d'Ivoire that used probit estimation found that immediate exclusive breastfeeding for up to six months had a favorable and strong effect on the likelihood of a child's survival.36 Children who were not breastfed in South Africa had a significantly higher risk of dying before turning five than those who were; some of the reported reasons for not breastfeeding included a lack of time due to mothers' work habits and related to sickness/diseases that would put the babies at risk if they breastfed.37
A study from Ethiopia showed that breastfeeding had a strong and significant effect on under-five child mortality.11 Further studies carried out in Ethiopia revealed that children who were not breastfed had a higher likelihood of dying before their fifth birthday.10,31 This might be due to breast milk's antibacterial and anti-inflammatory qualities, which protect against infection. This may also be due to the effects of unhygienic food preparation and feeding practices on children fed other than breastmilk.
Shorter intervals between births (below 24 months) were found to be strongly associated with an increased risk of under-five child mortality. These findings concur with those of other studies in the field. According to Indonesian multilevel survival analysis, under-five children with a previous birth interval of 24 months or more had a reduced death risk than those with a previous birth interval of fewer than 24 months.38 According to a study conducted in the SSA region, children under the age of five with preceding birth interval of less than 18 months and between 18 and 23 months had a ninety percent and fifty-five percent higher risk of death, respectively, than children born at 24 or above months interval.14
In Nigeria, children born with birth intervals of less than 24 months were more likely to die before their fifth birthday compared to those with a birth interval of 24 or more months.12 Similar findings were made in Ethiopia, where short birth spacing was proven to be a powerful predictor of under-five child mortality.32 This evidence might be a result of births being spaced out properly, giving the family more time to build their capacity to give the child the finest care possible on an emotional and financial level. Another possibility is that mothers who waited longer than 18 months between pregnancies would have recovered most of their body's nutrients and the blood they lost while carrying and nursing their first child.16
The risk of death before the age of five was found to be higher in children born to mothers who identified as Muslims. A comparable study carried out in rural Ethiopia provides evidence in support of this conclusion.30 The results of this study could be explained by the fact that more than half of the survey respondents (51.7%) were Muslims, increasing the probability and contributing to the study's findings. This result, however, conflicts with a related Nigerian study.39 This might be as a result of the Nigerian study using Christianity as a point of reference. But in this study, the Orthodoxy, a subset of Christianity, served as a reference group. The Nigerian study used information from the 2013 Nigerian Demographic and Health Survey, particularly from the northern part of the nation. Therefore, additional in-depth research is required to fully understand the situation of religious differences in child mortality.
One of the factors that are known to affect the mortality of children under the age of five is the use of ANC. In previous studies, the association of antenatal care utilization with lower childhood mortality has been documented.9,34 Mothers who utilize ANC services appropriately might have the right information regarding proper infant feeding practices and neonatal danger signs to advance a child’s health and prevent infections. Moreover, those mothers are more likely to attend PNC and immunization services, which are crucial for preventing, identifying, and promptly addressing several common childhood health issues. In this study, ANC utilization did not, however, associated with the mortality of under-five children.
In conclusion, this study's findings broadly concurred with those of the studies we've just examined. Furthermore, the findings of this study on birth interval align with the WHO’s recommendation of waiting at least 2 years after a live birth for birth spacing.40 Breastfeeding is often considered a preventive measure against child mortality around the world.
After accounting for cluster-level shared frailty, this study found that the estimated variance of the random effect (frailty factor) was θ = 0.41 with a p-value = 0.047. This indicates that there is sufficient evidence to support the existence of hidden heterogeneities between clusters.
This study analyzed a large, nationally representative sample of all deaths in Ethiopia. The study results were representative of all the regions. Additionally, this study incorporated a cluster-shared frailty component in the analysis. As a stand-in for cultural factors, this study used the religious affiliation variable.
Despite the above strength, the data set was subject to possible data collection error (i.e., only alive women aged 15-49 were interviewed); Thus, no data were available for children whose mothers were dead. Some determinants like cultural practices, and health professional-related factors were also unavailable. Data were collected cross-sectional by self-reported interviews which might be prone to recall and social desirability bias.
This study demonstrated that the mean survival time of under-five children in Ethiopia has increased. The risk of death is higher at a younger age and gradually decreases as one approaches the age of five. The statistically significant factors predicting under-five child deaths were preceding birth interval, family size, birth order, breastfed history, and religious affiliation.
Thus, it is recommended that health policies should focus on keeping the spirit of the continuum of care to improve children’s health. Facility-based care should be linked to home-based infant care visitations, which provide an opportunity for increasing immunization uptake, early diagnosis of danger signs, management of newborn and childhood illnesses, and prompt referral to an appropriate health facility.
Healthcare programs should put a strong emphasis on efforts to space out births and improve the health of the family. Healthcare providers should intervene in the community to maximize optimal infant and young child feeding practices.
Although this study showed that there were additional, unmeasured factors that contributed to the aggregation of under-five mortality in some clusters, more in-depth studies need to be done to identify the factors that resulted in the heterogeneity of the clusters in Ethiopia.
The authors would like to thank the Measure DHS Project for their free access to the original data of the 2019 Mini Demographic and Health Survey of Ethiopia.
H.Z.A. conceived the study, participated in its design and coordination, initiated the research, carried out the statistical analysis, interpreted the results, and wrote the final manuscript, critically reviewing it. B.T.O. and M.A. participated in the study’s design, guided the statistical analysis, and critically reviewed the manuscript. A.A.D., H.I.G., T.K. and were involved in principal supervision, participated in the study’s design and coordination, edited the manuscript, and critically reviewed the manuscript. The authors have read and approved the final manuscript.
The data sets recoded and analyzed during this study are available in the Measure DHS program repository to all registered users (https://www.dhsprogram.com/data/dataset_admin).
Ethics approval and consent to participate
Ethics review and participant consent was not required for this study because it used secondary data analysis of publicly available survey data from the measure DHS program. A written permission letter was taken from Institutional Review Board (IRB) of Demographic and Health Survey (DHS) program. The data has been used only for this registered research work, and it would not be passed on to other researchers.
This research work is funded by Salale University. The funders have no role in the study design, analysis, and decision to publish or preparation of the manuscript.
The authors declare that there are no conflicts of interest.

©2024 Abasimel, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.