MOJ
eISSN: 2381-179X


Case Report Volume 13 Issue 2
Yoshizawa Dermatology Research Clinic, Japan
Correspondence: Yusuke Yoshizawa, Yoshizawa Dermatology Research Clinic, KS Bldg. 2F 342-3 Katakura-Cho, Hachioji, Tokyo 192-0914, Japan, Tel +81-042-697-9923, Fax +81-042-697-6323
Received: May 06, 2023 | Published: May 17, 2023
Citation: Yoshizawa Y. A case of refractory acne vulgaris successfully treated with three color (blue, red, and infrared) LEDs as a substitute for isotretinoin. MOJ Clin Med Case Rep. 2023;13(2):38-41. DOI: 10.15406/mojcr.2023.13.00433
Objective: Acne vulgaris is a common chronic inflammatory disease of the skin. In the treatment of acne vulgaris, the first-line treatment (a 6- or 8-week trial of combined oral antibiotics and topical retinoid with benzoyl peroxide) fails, oral isotretinoin is recommended as additional therapy. However, it is necessary to prepare solutions other than isotretinoin in advance, because isotretinoin is a teratogen and has other undesirable effects. Blue and red light-emitting diodes (LED) irradiation is a well-established treatment for acne vulgaris with the antibacterial and sebocytes inhibitory effects. However, it has not yet been considered whether LED therapy is equivalent to isotretinoin therapy. In this report, treatment with blue, red, and infrared LEDs was used as additional therapy instead of isotretinoin in a patient with refractory acne vulgaris, and the efficacy was evaluated.
Methods: LED irradiation was performed once a week for 20 minutes. The whole of his face including the mandibular lines was irradiated with blue (405–415 nm), red (620–630 nm), and infrared (850 nm) LEDs simultaneously, using a N-LED 5000DK (Aderans Medical Research Co., Ltd., Tokyo, Japan). The integrated illuminance of each LED was as follows: blue, 4.72 J/cm2; red, 2.63 J/cm2; and infrared, 6.61 J/cm2.
Results: The improving changes of skin lesion was confirmed 4 weeks after the starting LED therapy, and the oral minocycline was able to be discontinued. Eight weeks after the starting LED therapy, the skin lesions revealed more significant improvement even after discontinued minocycline.
Conclusion: Red and infrared LEDs have inhibitory effects on toll-like receptor 2, a novel target factor in the treatment of acne vulgaris. It may be becoming clear that blue, red, and infrared LED therapy is much more involved in acne vulgaris than previous concepts that rely on antibacterial and sebum-suppressing effects. If this report triggers research on LED treatment for refractory acne vulgaris further, evidence may be obtained whether it is as effective as isotretinoin.
Keywords: isotretinoin, light-emitting diodes, refractory acne vulgaris, substitute, therapeutic
C. acnes, Cutibacterium acnes; LED, light-emitting diode; P. acnes, Propionibacterium acnes; TLR-2, toll like receptor 2
Acne vulgaris is a common chronic inflammatory disease of the skin. It is found in about 80% of young adults and adolescents. It is a disease that affects the pilosebaceous units of the skin and may result in inflammatory or non-inflammatory lesion.1-3 The four main pathological factors involved in the development of acne are the increased sebum production, irregular follicular desquamation, Propionibacterium acnes (P. acnes) proliferation and inflammation of area.4,5 Dysregulation of the cutaneous microbiome is also thought to play an important role in acne vulgaris.6,7 In the protracted inflammation of acne vulgaris, P. acnes triggers inflammatory cytokine responses by activation of toll-like receptor 2 (TLR-2).8
Acne has been recognized as a chronic disease, and therefore maintenance therapy has been deemed necessary to prevent acne recurrence.9 Topical benzoyl peroxide (BPO) and retinoids have been shown to effectively control acne and prevent relapse unlike antibiotics, which have been shown to be ineffective in preventing the development of the subclinical precursors of both inflammatory and non-inflammatory acne lesions.10 The group adopted the Acne Consensus Conference recommends that patients may be treated with topical medications including retinoids, BPO, salicylic acid, a combination of retinoid and BPO, or a combination of retinoids and BPO with or without antibiotics for mild acne; topical retinoid with topical BPO and a oral antibiotic for moderate acne.10 In general, the first-line treatment (a 6- or 8-week trial of combined oral antibiotics and topical retinoid with benzoyl peroxide) fails, another therapy is recommended as additional therapy.9
To reduce resistance and improve efficacy, oral antibiotics should be combined with topical BPO or retinoids in the treatment of refractory acne vulgaris. Furthermore, the duration of treatment should not exceed 12 weeks whenever possible.11,12 One particular drug for emergencies is isotretinoin.11 Only oral isotretinoin has a mechanism of action that reaches all the pathogenic relating to acne vulgaris. It is most effective drug available against acne with remission rate of 85% and higher.13 Isotretinoin has action that explicated on the sebaceous glands, decreasing their size and secretion, and also has anti-comedogenic activity and reduces the proliferation of Cutibacterium acnes (C. acnes).11 C. acnes is the main cause of inflammation in acne vulgaris. C. acnes secretes lipolytic enzymes that break down lipids in sebum, and free fatty acids produced at that time promote inflammatory reactions.14 However, caution should be exercised in early use in mild cases due to serious side effects, mainly associated with isotretinoin.13,15 Oral isotretinoin treatment lasts 16 to 24 weeks, but regular check-ups are necessary as side effects can occur. Also, isotretinoin is teratogenic and should not be taken during pregnancy or breastfeeding.16,17 Other undesirable effects include depression, irritable bowel syndrome, bone weakening, increased sensitivity to the sun, Stevens-Johnson syndrome, cheilitis, vomiting, nausea, and so forth.15-20 Isotretinoin may not be used because of its adverse effects or patient refusal of the treatment. In Japan, isotretinoin is not yet covered by insurance. It is necessary, therefore, to prepare solutions other than isotretinoin in advance in the treatment of refractory acne vulgaris.
Light-emitting diodes (LED) therapy is a well-established treatment for acne vulgaris.21 LED has antibacterial effect in blue LED,22,23 sebocytes inhibitory effects in blue and red LEDs.24 In the clinical trial report, severe acne shows a marginally better response than mild acne.21,25 At this point, LED therapy is not considered equivalent to isotretinoin therapy. However, red and infrared LEDs have inhibitory effects on toll-like receptor 2, a novel target factor in the treatment of acne vulgaris.26,27 It may be becoming clear that the therapy with blue, red, and infrared LEDs is much more involved in acne vulgaris than previous concepts that rely on antibacterial and sebum-suppressing effects.
However, when LED therapy is performed for the purpose of suppressing TLR-2, a new target factor for the treatment of acne vulgaris,26,27 it is speculated that LED therapy will exert a greater effect than previously thought.
In this paper, the author selected therapy with blue, red, and infrared ELDs irradiation as an additional therapy instead of oral isotretinoin for a patient with severe, refractory acne vulgaris, and reported the results with some discussion.
A 19-year-old man visited the author's clinic for refractory acne vulgaris. When he was in high school near his home, he had acne, but it was mild. Later, when he started commuting to college by train, his acne vulgaris began to worsen. He had no obesity, diabetes, or other endocrine disease. His skin lesions had appeared 6 months before coming the author's clinic, and had not responded to a 3-month regimen of oral roxithromycin and topical benzoyl peroxide in the primary care clinic. At the first day of the author’s clinic, dermatological examination showed well-demarcated erythema and aggregated pus-filled red papules with congregated comedones on the cheeks, mandibular lines, forehead, and nose. Several nodules were clustered on the mandibular lines (Figure 1a). The results of blood examinations, including serum androgen levels, were within normal limits. Severe acne vulgaris with nodules was diagnosed.9 Topical benzoyl peroxide with adapalene and 100 mg/day oral minocycline were started at the first day. This treatment was started on the first day (week 0). At the 3rd week, the skin lesions were aggravated, then an additional 15 mg/day oral prednisolone was prescribed for 2 weeks. However, since the exacerbation of skin lesions from the first visit continued to worsen until the 8th week (Figure 1b), LED therapy was started as an additional therapy.
LED irradiation was performed once a week for 20 minutes. The whole of his face including the mandibular lines was irradiated with blue (405–415 nm), red (620–630 nm), and infrared (850 nm) LEDs simultaneously, using a N-LED 5000DK (Aderans Medical Research Co., Ltd., Tokyo, Japan). The integrated illuminance of each LED was as follows: blue, 4.72 J/cm2; red, 2.63 J/cm2; and infrared, 6.61 J/cm2. In this treatment, one course was set to 2 weeks, and additional irradiation was performed while examining the symptoms. Because excessive LED irradiation may induce reactive oxygen species28 and promote inflammation, skin symptoms were carefully observed every week. Furthermore, LEDs, especially blue LED, have phototoxicity on retina,29,30 we always closed the eyes or wore light-shielding glasses during the treatment.
The improving changes of skin lesion was confirmed at the 12th week (4 weeks after the starting LED therapy), and the oral minocycline was able to be discontinued. The skin lesions revealed more significant improvement at the 14th week (6 weeks after the starting LED therapy) even after discontinued minocycline (Figure 1c). LED therapy was tolerated well, and the acne was successfully controlled by monthly irradiations alongside a topical treatment from the 16th week, although severe hypertrophic and atrophic scars developed on the mandibular lines and the cheeks, respectively.
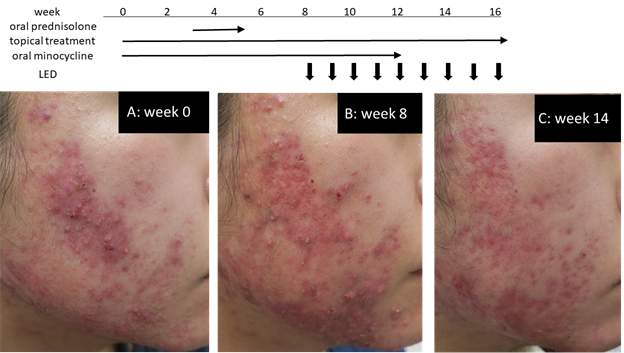
Figure 1 Clinical findings; (a) Week 0 (the first clinic visit): well-demarcated erythema and aggregated pus-filled red papules with congregated comedones were observed on the cheeks, mandibular lines, forehead, and nose. Nodules were concentrated on the mandibular line; (b) Week 8 (8 weeks after therapy with oral minocycline and topical benzoyl peroxide and adapalene): skin lesions were increased and severely developed; (c) The symptoms were improved after 4 weeks of three-color LED therapy (at week 12), and oral minocycline was ended. At week 14, the skin lesions were significantly improved.
Regarding the etiology of acne vulgaris, we have learned various things other than the four etiological factors mentioned in above. For example, treatment targeting TLR-2 for acne vulgaris may be useful in eliciting more effective therapeutic effects by adding to the conventional treatments.26,27
An inflammatory cytokine response of acne vulgaris is via activating toll-like receptor 2 (TLR-2), and an anti-TLR-2 antibody can inhibit the production of cytokines.26 TLR-2 expression is increased in the sebaceous glands of adult female acne lesions, and the expression of TLR-2 was significantly reduced after treatments with an oral contraceptive or a 15% topical azelaic acid gel, both of which resulted in clinical improvement.27 These studies have shown that the inflammatory responses in acne vulgaris are mediated by TLR-2, and the data have contributed to a better understanding of acne treatment.27
LED therapy has been used for acne vulgaris based on its abilities of the antibacterial effects by blue light22 and the sebaceous-inhibitory effects by blue and red lights.24 Low level red LED also inhibits hyperkeratinaization and inflammation in an in vitro model mimicking acne.31 Furthermore, exposure to LED light at red and near infrared (940nm) results in the downregulation of TLR2 in normal human epidermal keratinocytes.32 From these reports, simultaneous irradiation of blue, red, and infrared LEDs makes expectation of the effect of suppressing inflammation via TLR2 as well as sebaceous inhibitory effects in addition to the effects of oral antibiotics and topical BPO/adapalene. In fact, exposure to infrared LED light improved P. acnes-induced inflammation in a mouse model.33 Furthermore, infrared LED is expected to exert anti-TLR-2 effects to deeper areas by its longer wavelength.
A review of the combination of blue and red LED therapy for acne vulgaris21 reported twice weekly LED irradiation (blue: 7.2–48.0 J/cm2 and red: 9.6–120.0 J/cm2) or twice daily irradiation (blue: 0.91 J/cm2 and red: 1.22 J/cm2). This time, the intermediate output of the N-LED5000DK was chosen, which has three output settings. This irradiation was performed for 20 minutes once a week, and the integrate illuminance each session was shown as follows: blue; 4.72 J/cm2, red; 2.63 J/cm2, and infrared 6.61 J/cm2. In the presented case, the skin lesions showed improvement after 4 weeks, and clear improvement after 6 weeks (Figure 1c) of the LED therapy, respectively.
Recently, the author reported the efficacy of LED therapy in the treatment of lupus miliaris disseminatus faciei34 and rosacea.35 In the treatment for LMDF, blue, red, and infrared LEDs were irradiated to target tumor necrosis factor, a molecule related with the development of LMDF. For rosacea, blue and red LEDs were used to target LL-37 (cathelicidin), a critical molecule involved in the development of rosacea. LED therapy that aggressively targets molecules such as tumor necrosis factor, LL-37 (cathelicidin), or TLR-2 may be a more effective method in the treatment of skin diseases than previously thought including in the treatment of acne vulgaris.
In summary, although it was suggested that the LED therapy may serve as a substitute for oral isotretinoin, this report is a single case report without a matched control group. Ideally, it would be possible to adjust the irradiation intensity of each of the blue, red, and infrared LEDs and verify which combination is the most effective. If this report triggers research on LED treatment for severe, refractory acne vulgaris, evidence may be obtained whether it is as effective as isotretinoin.
None.
The author has no conflict of interest to disclose.

©2023 Yoshizawa. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.