Advances in
eISSN: 2378-3168


Review Article Volume 9 Issue 1
Scientist and CEO at Virtual Personal Trainer, Granada, Spain
Correspondence: JM Peregrin-Alvarez, Scientist and CEO at Virtual Personal Trainer, Granada, Spain
Received: January 24, 2019 | Published: February 26, 2019
Citation: Peregrin-Alvarez JM. Consistent weight loss linked to higher meal frequency. Adv Obes Weight Manag Control. 2019;9(1):12-14. DOI: 10.15406/aowmc.2019.09.00267
Obesity is a very interesting topic of study as it is directly related to human disease. Recently, we have reported that successful weight loss programs should consider the optimal timing for the brain control of weight-presetting, the fundamental of the “Lipostat theory”. This previous study was the first reported long-term human self-experiment involving successful weight loss, metabolic adaptation and weight-presetting, consistent with this theory while raising new concepts, ideas and setting up the bases for further investigations. One of such investigations is here in reported. An inverse relationship between people's habitual frequency of eating and body weight was consistently observed, suggesting that “snack-eating” may help to avoid obesity, further supporting other previously published meal frequency studies.
Keywords: obesity, overweight, ideal weight, weight loss, weight management, meal frequency, lipostat theory
BMI: body mass Index; HA: healthiest area; IW: ideal weight; M: milestone; MF: meal frequency; WG: weight gain; WL: weight loss
Obesity has been a global topic of concern for a long time as it is directly linked to human disease, causing more than 3.4 million deaths all around the word.1–3 To avoid this serious health issue, successful weight management programs should consider the required timing for feedback signals originating in adipose tissue to influence the brain centres that control eating behavior and activity (metabolic and motor),the fundamental of the “Lipostat theory”,4 which has been demonstrated for the very first time in humans in our previous study.5 This theory refers to the control of long term appetite, responsible for the control of body weight. As fat deposits accumulate, satiety signals are sent to the hypothalamus in response in an attempt to suppress the feeling of hunger and maintain a constant body weight. The study showed that HA was more efficient than simple BMI measurements, and the subject under study, originally obese, able to successfully reach and maintain an HA category (IW) over the years. New concepts and ideas were raised by that study, setting up the bases for further experimental validations. Thus, continuing with that study, the purpose of this case report is to present and discuss our self-experimental research on meal frequency over a long period of time with respect to changes in body weight.
A single individual was subjected to case study. The values of BMI Normal category were transformed into IW, based on height and weight, and further sub-categorized5 into the following categories: HA, BMI normal; and BMI Under weight. Two MF plans repetitions were implemented over a period of more than one year, organized into four milestones (M1-M4): M1, 16 weeks (~4 months) following a 3 meals/day plan; M2, same period of time following a 6 meals/day plan; and M3 and M4, by repeating M1 and M2 experiment under the same conditions. All milestones were energy balanced for weight maintenance purposes (calorie in: 2300kcal/day; calorie out: 500kcal/day). Any choice of food/activity was allowed following basic nutrition guidelines.7 HA and energy balance calculations, as well as calorie in (meals)/out (workouts) self-monitoring was done by mobile apps.8
Starting at weight 64, 5 kg (Figure 1) (height 178 cm) (HA; BMI category normal), a consistent and constant WL was recorded during M1 and M3 (average WL rate ~0.25kg/week), and a WG (average WG rate ~0.3kg/week) during M2 and M4. This represents an average total WL of 4.4 kg during M1 and M3, and an average total WG of 4.8 kg during M2 and M4. Milestones implementation provided with a robust and efficient way of gradually controlling a person's weight while costing less than conventional treatments.9 Small up/down peaks along the WL/WG lines correspond to metabolic adaptations. Interestingly, the HA trend was always shortly and consistently recovered after switching from a 6 to anusual 3 meals/day plan. These findings suggest WL due to a higher MF under controlled energy balance. This consistent inverse relationship between frequency of eating and body weight was observed by self-experimental validation (experimentation in which the experimenter conducts the experiment on her- or himself) and over a long period of time (more than one year), further supporting previous short-term MF epidemiological studies.6,10 Thus, our study suggest that “snack-eating” or small frequent meals, also referred to as grazing, picking or nibbling, may help body weight control, thus helping to avoid obesity and the implementation of effective weight management programs. However, since only one subject was subjected to study our conclusions should be taken with caution.
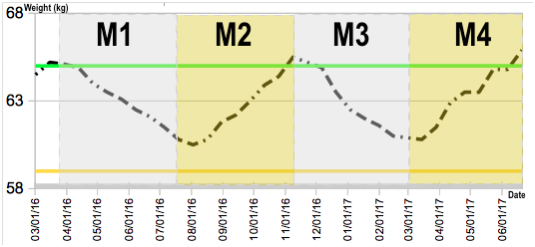
Figure 1 MF and weight control
Light grey coloured areas (M1/M3) correspond to 6 meals a day MF plans, and yellow areas (M2/M4) to 3 meals a day MF plans. The lower orange line represents the Underweight BMI line for the subject under study, and the upper green line represents HA (the healthiest weight area). The dashed black line shows consistent WL over M1/M3, and WG over M2/M4, related to MF. The consistent more than one year long pattern was observed throughout the complete duration of the self-experiment. A low HA-presetting was chosen by personal preference, suggesting that a personal control of body weight is possible after a successful weight-presetting, further supporting our previous find ings.5
It has been hypothesized that eating small frequent meals enhances fat loss and helps to achieve better weight maintenance. A number of observational studies lend support to this hypothesis, with an inverse relationship noted between the frequency of eating and adiposity.6,10 However, these studies were performed over short periods of time, thus being questioned or considered weak by other conflicting studies.11–13 Our study represents the first successfully consistent long-term weight control self-experiment suggesting that “snack-eating” may help WL programs, thus helping to avoid obesity/overweight while controlling cholesterol levels and reducing cardiac risk.14 Proposed mechanisms that could explain this phenomenon include the favourable effects of increased MF on improved glucose homeostasis.15–17 and increase in the thermal effect of feeding.18,19 Furthermore, frequent eating, either regular meals or between-meal snacks, may prevent from overeating at mealtime (appetite control).20–21 People eating only a few times a day have elevated 24-hour insulin levels. High insulin levels promote storing energy in body fat; and high insulin level is also a marker for heart disease risk. Moreover, once again, we have demonstrated the affectivity of combining technology and personal science. Mobile technology allowed a close interaction, autonomy and help motivation.5 This study set up the bases for the systematic implementation of efficient weight management programs. With sufficient funding these results can be adapted and reproduced on larger groups. Future studies should be able to further validate these results and answering some interesting questions raised here such the role of culture in body weight as MF might be determined by certain cultures.23–30
None.
The authors declared there is no conflict of interest.

©2019 Peregrin-Alvarez. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.