Advances in
eISSN: 2378-3168


Research Article Volume 10 Issue 6
School of Sport and Exercise, University of Gloucestershire, UK
Correspondence: CD Mills, School of Sport and Exercise, University of Gloucestershire, Oxstalls Campus, Gloucester, Gloucestershire, GL2 9HW, UK
Received: November 17, 2020 | Published: December 11, 2020
Citation: Mills CD, Wellington HB. The impact of a 6 week walking intervention on an obese population in relation to walking distance, waist to height ratio and body mass index. Adv Obes Weight Manag Control 2020;10(6):181-189. DOI: 10.15406/aowmc.2020.10.00326
Obesity is a health condition, often resulting from an imbalance between physical activity and calorie intake and while invasive and intense interventions may be necessary for some obese individuals (OI), changes in activity and lifestyle over long periods of time are arguably the safest, most sustainable solution. High Intensity Interval Training (HIIT) has been widely observed to increase rapid fat oxidation in obese populations (OPs), it conversely increases health risks for OIs who often have limited cardiovascular fitness, increased joint loading and high blood pressure. However, submaximal aerobic exercise, such as walking, can be used as an initial intervention for OI who lead sedentary lifestyles, to reduce weight and increase aerobic capacity in an arguably safer way. Therefore, the aim of this study was to investigate the effect that a submaximal walking intervention has on anthropometric measures in an OP.
Methods: The experiment had a within-group, longitudinal design with repeated measures on n=6 participants aged 34-54 (M=50.3, SD=8.02, 66.7% female) who walked 30 minutes daily over a 6-week period. All participants were classified as obese at week one of the intervention period, and as such were required to have a body mass index (BMI) >30 and a waist to height ratio (WHR) of >0.58 or >0.54 for men and women, respectively. Anthropometric measurements recorded at weekly intervals throughout the intervention included BMI, WHR, Waist Circumference (WC) and body mass (BM).
Results: A non-parametric Friedman Test was carried out using SPSS and a statistically significant difference in BM (pre-93.34; post–87.86, diff–5.48kg), BMI (pre-31.38; post–29.58, diff–1.80), WHR (pre-.61; post–.56, diff –.05), WC (pre-39.34; post–37.26, diff–2.08inches (")) was observed before and after the 6-week intervention (P<0.001). Post Hoc analyses using a Paired Samples t-Test confirmed the statistically significant effect of 30 minutes of daily walking on all measures over the 6-week period (p<0.05) (pre-2.63; post–2.89, diff–.26 km) with average distances reaching 2.7km.
Conclusion: Results found the prescribed 6-week walking intervention caused a significant reduction in BM, BMI, WHR and WC and an overall increase of distance walked by participants. Moreover, can be concluded that submaximal exercise can benefit OIs by reducing all areas explored whilst keeping the risk of a health implication to a lower level than HIIT.
Keywords: obesity, intervention, walking, body mass index, waist to height ratio
Obesity is a health condition defined as a Body Mass Index (BMI) >30 (National Health Service, NHS), which often results from an imbalance between physical activity and calorie intake. Abnormal or excessive fat accumulates forming adipose tissue, often impairing physical and psychological health.1 Obesity is a significant problem in society, being classed as a worldwide epidemic,2 that must be urgently addressed as obesity statistics continue to increase yearly.3 This increase is putting health organisations under significant financial pressure, with an estimated projection to reach £9.7 billion in the United Kingdom by 2050.4 This outlay is unsurprising since figures estimated 68% of males and 60% of females were classified as overweight or obese in 2019. Obese individuals (OI) are 28% more likely to develop Cardiovascular Disease (CVD) than those with a healthy BMI5 further adding to financial strain.
There is a clear need for comprehensive, achievable, and clinically validated physical interventions to address this societal problem and alleviate strain on the NHS. Despite the psychological and physical benefits of daily exercise and the comprehensive research available reporting the benefits of high intensity interval training (HIIT), the impact of submaximal exercise on health in both healthy and obese populations (OP) has received limited research. Specifically, the impact of daily, submaximal walking on the physical measurements of OPs is not widely documented. HIIT and intense aerobic training has been widely observed to have a positive effect on weight loss in OPs by optimising fat oxidation.6 However, at high intensity training levels OPs are at an increased risk of other negative health implications such as myocardial infarction7 and anatomical injuries. There is debate in recent literature as to whether HIIT is most effective for weight loss and compliance in OPs. HIIT is characterised by short repetitions (30s-1min) of intense exercise (>80% maximal capacity) alternated with periods of rest.8 Shiraev and Barclay9 suggested HIIT had beneficial qualities for ‘at risk’ populations attempting body mass loss, identifying an association with compliance and rapid improvements in cardiovascular fitness and metabolic rate. Further support for HIIT was found by Türk et al.,10 when conducting a meta-analysis of randomised control trials between 2000-2017. The research studied the effect of HIIT in OPs in comparison to a low intensity control.The authors found HIIT to have superior qualities to ‘traditional exercise’ when trying to improve cardiopulmonary fitness and reduce weight by increasing fat oxidation.
While invasive interventions may be necessary for individuals whose weight pose significant health risks to life, changes in activity and lifestyle arguably remain the most beneficial long-term solutions for reducing obesity in a sustainable and safe way. It is important to identify clinically validated interventions to assist weight loss in OPs whilst ensuring physical health and safety. Opposing research to HIIT interventions, identified submaximal efforts as a key type of exercise for initial body mass loss in OPs, as it can be completed at lower intensities and requires lower levels of cardiovascular fitness.11 For instance, O’Dennell and Hasselbring12 suggested OI may not have the physical capabilities to participate in any high intensity exercise due to significant health risks including MI and damage to joints due to excess weight. In a study completed by Blüher et al.,13 biochemical markers were present, including those related to insulin resistance, for OI the continuous physical strain placed on vital organs during HIIT often results in an increased mental barrier compared to healthy individuals.14 Consequently, it is not recommended that individuals with large amounts of excess body fat participate in intense exercise.15 These individuals, who are likely to be sedentary, should consider light aerobic exercise for longer periods for optimal weight loss while ensuring minimal health risks.16 Babb et al.,17 compared the effect of submaximal exercise on obese women (fat 35% +/-5%) and lean women (fat 22% +/-2%). They found that the VO2, pulmonary ventilation during exercise and heart rate (HR) of obese women increased significantly more than those classified as lean (p<0.05).These results confirm OI cannot complete exercise at the same level as individuals with a ‘healthy’ body mass index (18.5 – 24.9). However, further research is required in male populations to allow generalisability.
Walking as a specific type of submaximal exercise that can be carried out by OPs to aid weight loss. Kaur et al.,1 carried out a 12-week intervention on n=30 OI (BMI >30kg/m) aged 20-40, classified as having a sedentary lifestyle. Participants walked daily for 12 weeks and measurements of BMI and waist-hip ratio were collected bi-weekly. Results indicated a significant decrease in BMI and waist-hip ratio because of the intervention. Walking, therefore, has been used as an initial intervention to reduce body mass, increase aerobic capacity, and therefore reduce the risk of myocardial infarction during higher intensity exercise once an intervention is completed.18 This increases the likelihood of the participant losing body fat through fat oxidation in a controlled and safe manner before attempting high aerobic exercise. Therefore, the purpose of this study was to explore specific measures of BMI, body mass (BM), waist to height ratio (WHR) and waist circumference (WC) at weekly intervals. For this study obesity is defined as a BMI >30 and a WHR of >0.58 for men and >0.54 for women, respectively. Furthermore to explore the impact of a short term 6-week walking intervention on an OP by hypothesising that (1)Average BM, BMI, WHR and WC will significantly decrease over the 6-week period due to the walking intervention and (2) average distance walked will increase over the 6-week period due to the walking intervention.
Participants and recruitment
n=6 participants aged 34-54 (M=50.3, SD=8.02, 66.7% female) were recruited via telephone and information letter using opportunity sampling in the community. To qualify for participation, female and male participants were required to have a WHR of >0.54 or >0.58 respectively, and a BMI of >30.1 Recruited participants had taken early retirement or worked a deskbound employment and therefore classified themselves as sedentary, as defined by Grimby et al.,19 Participants completed a health questionnaire to identify whether the participant had any underlying health conditions that prevented them completing the intervention. Therefore, it was vital that participants had no significant underlying health conditions, due to the risks associated with increasing activity levels from sedentary to active in OPs. National Health Service (NHS) guidelines were followed, such that the participant informed their GP before completing the intervention.Steps were taken to assess whether current fitness levels and individual circumstances would allow completion of the intervention without significant risk to their health. An information sheet and informed consent were provided, and all participants were debriefed pre and post participation. The email address of the head researcher was provided to allow participants to ask questions throughout the 6-week period. Data was stored on a password protected laptop ensuring secure storage of information (Data Protection Act, 2018) and approved by the University’s research ethics committee.
Procedure
Prior to this start date the head researcher completed a series of pilot studies to ensure International Society for the Advancement of Kinanthropometry (ISAK) protocols were followed to the highest of standards and chances of human error were reduced. Anthropometric data collection followed protocols set by ISAK20 to ensure strict adherence to the accuracy and precision of each measurement whilst maintaining privacy and comfort to participants.21 These included taking measurements in the comfort of their own home and the option to wear light clothing if they felt uncomfortable. Finally, all participants were kept informed of the researcher’s actions before and during each measurement being taken. Measurements included body mass, stretched stature, waist and hip circumferences.
From this data, BMI and WHR were calculated (NHS, 2018). Participants were instructed to walk 30 minutes daily for 6 weeks at a rate of perceived exertion (RPE) of 11-14. RPE was monitored to control physical exertion which may have influenced the intervention success or resulted in a deviation from submaximal exercise. Each walk the participant completed was mapped using STRAVA and uploaded to a shared platform where both the researcher and participant could view the information. Perceived rate of exertion was also uploaded to the shared platform after each walk. At 7-day intervals BM and WC measurements were taken by the researcher and BMI and WHR calculated using the same methodology as the initial measurements. n=7 measurements were taken for each dependent variable throughout the experiment. The researcher had daily communication with participants throughout the intervention to ensure they were completing the exercise correctly and continued to be comfortable with the procedure (Figure 1).
Anthropometric measures
Body mass was measured using SECA digital scales (SECA gmbh and co Ltd, Hamburg Germany). Stretched stature was measured using a portable Stadiometer (SECA gmbh and co Ltd, Hamburg Germany). Waist circumference (WC) was calculated using a standardised Anthropometry flexible steel measuring tape.21 Waist to Hip Ratio (WHR) was calculated by dividing waist circumference by stretched stature. Body Mass Index (BMI) was measured using the NHS BMI calculator.4 This calculation included stretched stature (cm), body mass (kg), age, sex, and activity level information to calculate the BMI. Activity level is measured using a self-report scale. A BMI of >30 indicates obesity. All measures adhered to International Society for the Advancement of Kinanthropometry (ISAK) protocols.20,21
Walking data
Each walk completed by participants was tracked using STRAVA, GPS application. This ensured the collection of reliable and accurate duration, elevation, and pace data.22 STRAVA uses satellite information to track an individual whilst completing physical activity.
Borgs rate of perceived exertion scale
The Borgs self-report perceived rate of exertion scale was also completed by participants after every walk. The scale ranges from six to twenty, with a score of six indicating feelings of no exertion at all and twenty reflecting maximal effort.23 Individuals were asked to keep their RPE between 11 and 14 to imitate submaximal exercise. The RPE scale is subjective to an individual’s personal pain threshold.
Data analysis
Data was coded where necessary, checked for missing values, and exported from EXCEL Microsoft Software into IMB SPSS 24 software. Kolmogorov-Smirnov scores for homogeneity were found, Descriptive statistics were calculated with Non-Parametric Friedman Test and Post Hoc analyses (paired samples T-test) being the chosen tests for coded data. While six participants started the intervention, one participant only completed one week of the intervention and therefore their data was discounted from the analysis.
Kolmogorov-Smirnov scores for homogeneity of variance were insignificant (>.05) for all variables, suggesting parametric data assumptions were met. This is reflected in the choice of statistical tests used in the current analysis. Descriptive statistics for age, body mass, WHR, BMI, and WC both before and after the 6-week period are presented in Table 1. Descriptive statistics for average distance covered, time spent walking and RPE were collected for each participant over 6-weeks and are presented in Table 2 and visuals for distance walked (km) in Figure 2 and elevation gain (m) in Figure 3.
|
Variables |
M Before (n=5) |
SD |
Range |
M After (n=5) |
SD |
Range |
Diff |
|
Age (years) |
49.8 |
8.84 |
34.00–54.0 |
49.8 |
8.84 |
34.00–54.00 |
- |
|
BM (kg) |
93.34 |
7.26 |
87.00–105.00 |
87.86 |
6.92 |
79.90–98.20 |
5.48 |
|
WHR (cm) |
0.61 |
0.4 |
00.58–.66 |
0.56 |
0.02 |
0.53–0.57 |
0.05 |
|
BMI (kg/m2) |
31.38 |
1.84 |
30.00–34.60 |
29.58 |
2.52 |
27.00–33.70 |
1.8 |
|
Waist (“) |
39.34 |
1.89 |
38.00–42.00 |
37.26 |
2.25 |
35.20–40.30 |
2.08 |
Table 1 Descriptive statistics for age, weight, WHR, BMI, and WC before and after a 6-week period of walking for 30 minutes daily
|
|
Week 1 |
|
|
Week 2 |
|
|
Week 3 |
|
|
Week 4 |
|
|
Week 5 |
|
|
Week 6 |
|
|
|
T |
D |
RPE |
T |
D |
RPE |
T |
D |
RPE |
T |
D |
RPE |
T |
D |
RPE |
T |
D |
RPE |
|
|
1 |
30.52 |
3.07 |
12.86 |
30.41 |
3.09 |
15.71 |
30.37 |
3.07 |
15.29 |
30.42 |
3.31 |
14.86 |
30.25 |
3.25 |
16.14 |
30.32 |
3.35 |
15.33 |
|
2 |
30.05 |
2.35 |
14.29 |
30.01 |
2.36 |
14 |
29.91 |
2.36 |
12.86 |
29.61 |
2.3 |
12.57 |
27.57 |
2.11 |
12.71 |
28.24 |
2.15 |
12.43 |
|
3 |
29.95 |
3.02 |
11.86 |
30.12 |
3.15 |
12.57 |
30.32 |
2.99 |
11.57 |
30.54 |
3.05 |
11.57 |
30.17 |
2.93 |
10.86 |
31.48 |
3.08 |
11.29 |
|
4 |
29.86 |
2.2 |
11.29 |
29.9 |
2.24 |
11.43 |
29.92 |
2.11 |
10.71 |
30.67 |
2.45 |
11.71 |
29.81 |
2.61 |
11.86 |
31.62 |
2.85 |
12.5 |
|
5 |
30.12 |
2.54 |
11.29 |
30.15 |
2.57 |
10.71 |
30.26 |
2.6 |
9.43 |
30.05 |
2.63 |
10.14 |
29.81 |
2.61 |
11.86 |
31.62 |
2.85 |
12.57 |
Table 2 Average distance covered, time spent walking and perceived rate of exertion for each participant over the 6-week period
Key: T, time, D, distance, RPE, perceived rate of exerction
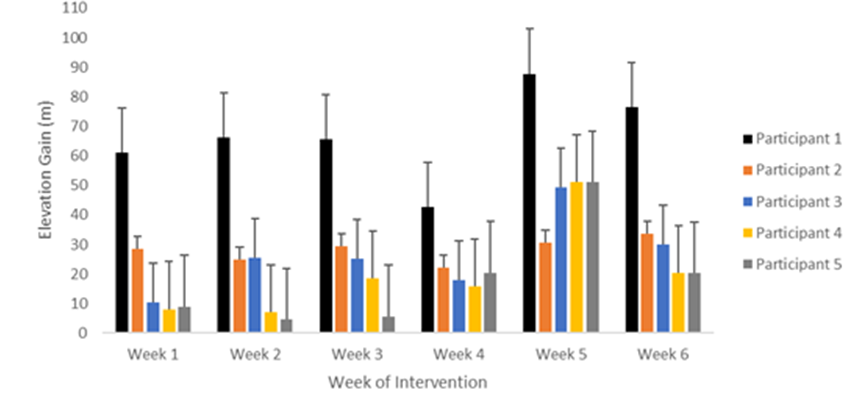
Figure 3 The elevation gain (m) of each participant at weekly intervals across the 6-week intervention.
To assess the effect of 30 minutes of walking on the dependent variables (weight, WHR, BMI, and WC) over a 6-week period, a one-way ANOVA was initially carried out. Mauchly's sphericity was severely violated and the decision was made to run a Friedman's Test for non-parametric data. Post hoc analyses were completed for initial and final measures of weight, WHR, BMI and WC using paired samples t-tests in order to further explore the significant effect found in the Friedman’s Test of 30 minutes of walking on the dependent variables.
Body mass
From the 30-minute walking intervention a statistically significant difference in mean weight was observed from weeks 1 to 6, X2(6)=29.66, p<.001. A paired samples t-test was conducted comparing the weight (Kg) figures before and after 30 minutes daily, 6-week walking intervention. On average participants had a higher weight before (M=93.34, SD=7.25) than after the 6-week intervention (M=87.86, SD=6.91). This decrease of 5.48 (Kg) (SD=2.57), 95% CL [2.29, 8.66], was statistically significant, t (4)=4.77, p.009 (Figure 4).
Waist to hip ratio
From the 30-minute walking intervention a statistically significant difference in mean WHR was observed from weeks 1 to 6, X2(6)=28.12, p<0.001. A paired samples t-test was conducted comparing WHR figures before and after 30 minutes daily, 6-week walking intervention. On average participants had a higher WHR before (M=.608, SD=.035) than after the 6-week intervention (M=.554, SD=.016). This decrease of .054 (SD=.023), 95% CL [.025, .082], was statistically significant, t (4)=5.24, p.006 (Figure 5).
Body mass index
From the 30-minute walking intervention a statistically significant difference in mean BMI was observed from weeks 1 to 6, X2(6)=29.31, p<0.001. A paired samples t-test was conducted comparing BMI (Kg/M2) figures before and after 30 minutes daily, 6-week walking intervention. On average participants had a higher BMI before (M=31.38, SD=1.84) than after the 6-week intervention (M=29.58, SD=2.52). This decrease of 1.8 (SD=.815), 95% CL [.78, 2.81], was statistically significant, t (4)=4.93, p.008 (Figure 6).
Waist circumference
From the 30-minute walking intervention a statistically significant difference in mean WC was observed from weeks 1 to 6, X2(6)=29.49, p<0.001. A paired samples t-test was conducted comparing WC figures before and after 30 minutes daily, 6-week walking intervention. On average participants had a higher WC before (M=39.34, SD=1.89) than after the 6-week intervention (M=37.26, SD=2.24). This decrease of 2.08 (SD=.454), 95% CL [1.51, 2.64], was statistically significant, t (4)=10.22, p<0.001 (Figure 7).
This study aimed to quantify the effects of submaximal exercise on an OP, specifically 30 minutes of daily walking over a 6-week period. This was done by collecting BMI, BM, WHR and WC at weekly intervals. As hypothesised the intervention was observed to significantly reduce BMI (kg/m2), BM (kg), WHR and WC (inches), with the most noted individual decrease in weight of 8.5kg for participant 4. Gender differences in the intervention impact were observed, with males showing greater decreases across the 6 weeks in all measures, apart from WC. Finally, distance walked in the 30-minute exercise period was shown to increase by an average of 0.3km over 6 weeks.
The increase in distance covered over the six-week period
While male participants covered a greater distance on average than females during the intervention, overall participants showed an increase in distance covered over the 6-week period. Figures 2&3 shows the average weekly distance walked and elevation gain. A negative relationship was observed between the two variables such that as elevation increased, distance walked decreased. Four of the five participants showed a large increase in walk distance average when comparing week 1 to week 6. The participant whose data did not conform to the observed trend reduced their average distance walked by 0.2km throughout the intervention period. However, when comparing the average elevation gain for each walk from weeks 1 to 6, this participant increased their elevation by 5 metres per walk which could explain the reduced distance covered. Furthermore, all participants showed a reduction in all physical measures of excess adipose tissue.
Since Goran et al.,24 observed submaximal aerobic capacity to be lower in an obese state when compared to a healthy state, as indicated by higher heart rate and % VO2max,it is possible that the increase in distance walked over the current intervention period could be a result of reduced body fat and increased aerobic capacity. While VO2max relative to fat free mass is likely to be identical before and after the intervention, as excess adipose tissue is lost, respiratory exchange ratio (RER) becomes significantly lower, increasing aerobic capacity.24 By changing activity levels from sedentary to active the current participants were able to reduce the relative demand on their respiratory system and increase their distance walked. In addition, fat loss can increase distance walked relative to the biomechanical effect that excess fat has on the body whilst walking. Browning &Kram25 found that an obese adult had a larger load through all lower limb joints whilst carrying out the walking motion, making it increasingly harder to walk the same distance as a healthy weighted adult. It could therefore be assumed that the increase in distance walked seen in the current study may reflect the fat loss by participants over the 6-week intervention period and the reduction in joint load. Fat loss and its implications for aerobic capacity and joint loading, as well as changes in elevation gain clearly influence distance walked in a set period. The present study shows the positive benefits of submaximal activity on a previously sedentary OP and their respiratory efficiency and ability to exercise.
Submaximal exercise as a positive intervention for obese populations
Data collected over the 6-week intervention period showed a significant decrease in BM, WHR, BMI and WC in line with the hypothesis. While most previous research supports HIIT as an optimal intervention for rapid weight loss in Ops,10 the current results challenge this literature and highlights the importance of submaximal efforts for initial weight loss. The current results are supported by a longitudinal study conducted by Esposito et al.,26 who also explored the effects of daily submaximal exercise on an OP (n=120, females). Authors observed a significant decrease in weight and BMI over a two-year period. The present study extended the research of Esposito et al.,26 by recruiting male participants, thus showing that the effect is not restricted to females. Esposito et al.,26 also controlled the daily calorie intake of their participants. The current study did not control diet which may have influenced variability among weight loss of participants. Since Esposito et al.,26 conducted their study over two years with a similar methodology to the current study, the current results could be extended if the intervention period were increased. On the other hand, HIIT has consistently been identified as an optimal training method to reduce fat percentage in OPs. Zhang et al.,27 (n=43; females) compared the effects of HIIT with prolonged continuous submaximal exercise over a 12-week period. Authors identified submaximal training to have lesser effects on abdominal visceral fat reduction compared to 15 minutes of HIIT, stating HIIT to be the predominant strategy for controlling obesity due to its time efficiency. The present study did not compare the two training types and therefore no conclusive statements can be made around the benefits of one in comparison to the other, results showed the submaximal intervention to have significant effects on WC reduction and WHR. Previous research has also favoured submaximal exercise over HIIT for weight loss in sedentary OI. Keating et al.,28 reported results indicating greater benefit of submaximal exercise over HIIT for participants that had previously been sedentary. Participants completing the submaximal intervention showed significant decreases in trunk fat percentage (3.1%; SD=1.6), in line with reductions seen for WC and WHR in the present study.
Since participants in the present study also self-identified as sedentary prior to the intervention, it is possible that activity levels and physical health influence the effectiveness of HIIT in comparison to submaximal exercise. Since sedentary populations are more likely to have minimal aerobic capacity and an increased BMI, submaximal training is likely to incur fewer health risks. This is supported by Browning & Kram25 who found that a sedentary obese individual had a greater demand of relative cardiovascular fitness to complete the same exercise as a healthy individual. Their results suggest that walking at a comfortable, submaximal pace for a set distance may be a more appropriate for BM management in obese adults then high intensity exercise. Both HIIT and submaximal training increase fat oxidation29 and the current study illustrates the benefits of submaximal training for weight loss in OPs. Further research is required to identify the optimal approach to weight loss through an exercise intervention, while also considering the safety of patients who are likely to lead sedentary lives and have low cardiovascular fitness.
Gender differences in intervention impact
Submaximal exercise was shown in the current research to have a positive impact on body mass loss in an OP in just 6 weeks. However, gender differences in intervention success were identified. Average body mass loss in male participants (6.6kg) was observed to be greater than female participants (4.3kg). Donnelly and Smith (2005) identified similar gender differences for a similar programme completed over 12 weeks. The authors attributed this to the increased energy (KJ) expenditure, from males, during the same volume of exercise. Therefore, if diet remains consistent, the weight loss, through an exercise intervention, is likely to be greater in males. Gender differences in body mass loss may be attributed to physiological differences in energy expenditure during exercise. It is a common phenomenon that when exercise is increased, feelings of hunger along with calorie intake increase.30 As a result, weight loss may be less pronounced despite the implementation of a positive intervention.
In addition, gender differences in weight loss may have occurred due to a difference in average distance covered by males and females during the 30-minute period. Results indicating greater weight loss in males could be reflective of the average daily distance walked by each gender. Over the 6-week intervention males walked an average of 3.11km (Table 2) whereas females walked 2.44km (Table 2). These results show similarities to those found by Browning et al.,31 who suggested that males were able to exert less energy to cover the same distance as females. This physiological difference enabled male participants to walk 0.14km further than females in a 5-minute period. It is possible that the greater distance covered by male participants, in the present study, may be reflected in their superior weight loss. Finally, contrary to previous research suggesting that males often lose greater trunk fat than females due to exercise interventions, the current study indicated that females had a larger reduction in WC circumference than males over the 6-week intervention.
There was a significant decrease in WC for all participants through weeks 1 to 6 (P <0.001). Females had an average circumference reduction of 2.3” whereas males showed a reduction of 1.7”. Previous research identifies that body fat percentage and fat distribution differs between males and females.32 As stated by Karastergiou et al.,33 due to a difference in hormones, females store a significant amount of fat around the gluteus maximus, upper leg and pelvis area. Males predominantly store excess fat around the trunk and waist. This suggests that trunk fat reduction in obese, male participants should be greater than females, reflected by superior WC reduction after an exercise intervention.34 The current results, indicating greater WC reduction in females, contradicts the findings of Power & Schulkin34 and does not follow the standard research. The lack of consistency with previous research may be due to sample size (n=5) and its lack of representation of the true OP. While the ratio between men and women was 2:3, due to the sample size the effect of anomalies is greater. For example, if one female participant were significantly larger at the beginning of the intervention or lost significant weight from the trunk area, this would influence the results in a more pronounced way. Much of the research currently available in obesity literature focuses on female participants as the female body resists the loss of energy stores more than males. 30% of women are obese in the UK in comparison to 26% of males (2017).35 These statistics result in women often qualifying more readily for obesity research. However, it is important to further explore the effects of exercise interventions on male populations as obesity continues to rise in both genders.36–39
This study contributes to the growing body of evidence quantifying the benefits of submaximal exercise as an intervention for OPs. Results highlight the need to further explore gender differences in intervention effectiveness while also recruiting larger samples to ensure result reliability. Furthermore, by running clinical pilot trials for effective interventions and exploring gender differences in weight loss, health professionals can begin to prescribe specific and measurable programmes to support OPs in their initial weight loss strategy. Since obesity is rising and becoming a key concern in society, developing clinically validated interventions, which ensure the safety and compliance of OPs, is increasingly important. By doing so it is possible to reduce the pressure on the NHS by reducing obesity related illness, allowing vital resources to be invested elsewhere, improving the health of the population.
The study hypothesised that (1)Average BM, BMI, WHR and WC will significantly decrease over the 6-week period due to the walking intervention for n=6 participants. This study found to significantly reduce all measurements and suggested that a submaximal walking intervention does reduces these explored areas and (2) average distance walked will increase over the 6-week period due to the walking intervention. This study found that n=4 of the 5 participants increased walk distance over the 6 week walk intervention however, no scientific conclusion can be assumed as more in-depth research needs to be carried out on the effects of weight reduction on walking distance in an obese population.
None.
We disclose no conflicts of interest.
None.

©2020 Mills, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.