Journal of
eISSN: 2373-6410


Case Report Volume 9 Issue 6
Department of Neurosurgery, Hassan II University Hospital of Fez, Morocco
Correspondence: Marouane Hammoud, Medicine doctor, Department of Neurosurgery, Hassan II University Hospital of Fez, Morocco, University Sidi Mohammed Ben Abdellah, Fez, Morocco, Tel 00212661491896
Received: October 21, 2019 | Published: November 26, 2019
Citation: Hammoud M, Lakhdar F, Benzagmout M, et al. Cervical tarlov cyst mimicking spinal hydatid disease: case report. J Neurol Stroke. 2019;9(6):323-325. DOI: 10.15406/jnsk.2019.09.00397
Background: Perineurial (Tarlov) cysts are usually incidental findings during magnetic resonance imaging of the lumbosacral spine. The Cervical localisation have been reported to be a rare occurance. We are reporting a case where a high cervical perineural cyst was masquerading as a spinal hydatid disease.
Case presentation:We report a case of symptomatic cervical Tarlov cyst in a 9 years old girl operated on twice for pulmonary and hepatic hydatid cyst. Spinal magnetic resonance imaging (MRI) showed an extradural intraspinal lesion with fluid-equivalent signal extending from C5 to T2. Based on the history, the diagnosis of spinal hydatid disease was suggested. Surgical excision of the cyst resulted in significant improvement in patient symptoms, and histological examination revealed the diagnosis of a Tarlov cyst.
Conclusion: Cervical perineural (Tarlov) cyst can be symptomatic by causing nerve root compression and can be mistaken as a spinal hydatid disease on imaging. Surgical treatment can be curative.
Keywords: Tarlov cyst, hydatid cyst, diagnosis, management MRI, cervical spine.
TC, tarlov cyst; CSF, cerebrospinal fluid; MRI, magnetic resonance imaging
Tarlov cyst (TC) is defined as a cystic dilatation between the perineurium and endoneurium of spinal nerve roots, located at level of the spinal ganglion and filled with cerebrospinal fluid (CSF) but without communication with the perineurial subarachnoid space.1 It is most often found in the sacral spine with a prevalence of 4.6% in the general population with about 13% of those being symptomatic.1,2 The Cervical localisation have been reported to be a rare occurance,3 to our knowledge there are only five published cases of symptomatic cervical Tarlov cyst.4 Here in a case of symptomatic cervical TC that was masquerading as a spinal hydatid disease.
A 9-year-old girl, with medical history of surgery for pulmonary and hepatic hydatid cysts at age of 8, treated with anthelmintic with good outcome. As far as her past medical history is concerned, there was a history of cervical plexus trauma at the age of 6 with monoparesis sequelae of the left arm.
She presented with progressive left hemiparesis 4 weeks earlier. On clinical exam, all deep tendon reflexes were normal. Proximal muscle strength of the left leg and the ipsilateral upper extremity was 3/5. Electromyography (EMG) showed abolition of motor and sensory responses of nerves SPE and SPI on the left upper limb.
MRI of the cervical spine showed intraspinal cystic lesion of extra-dural location lateralized to the left, extending from C5 to T2 causing a stenosis of the adjacent foramina, without contrast enhancement of the cyst wall (Figure 1).
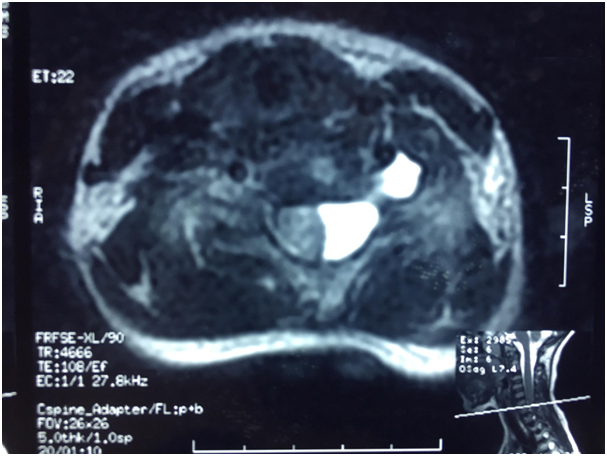
Figure 1 T2-weighted axial MRI showing an intraductal cystic lesion lateralized to the left and protruding in the adjacent neuro foramina. Squeezing the cervical spinal cord.
Based on the MRI finding and the history of patient, the diagnosis of spinal hydatid disease was suspected. The patient underwent a C4-T2 laminotomy (Figure 2), intraoperatively we found cystic lesions strongly adhered to the dural mater with an appearance that was evoking congenital cysts. At this point, we opened the capsule and a clear CSF-like liquid came out from the cyst, we conducted a careful excision with dural plasty.
The histological examination showed fibrous tissue and the presence of neural elements, which is typical for perineural cysts. Postoperatively, the patient has improved significantly her left lower-limb strength. A postoperative MRI of the cervical spine was performed after 6 months showed no recurrence of the cyst (Figure 3).
Tarlov cysts, or perineural cysts, firstly described by I.M. Tarlov in 1938 as an incidental finding during his autopsy studies of the filum terminale.5 They are pathological fluid collections located between the peri and endoneurium, filled with CSF, therefore the signal is cerebrospinal fluid (CSF)-like signal on all MRI sequences.6
They are often multiple and are mainly located in the sacral region, cervical location is rare. In a systematic study Burdan et al. reported about a prevalence of 1.2% of cervical perineural cysts.7 They are symptomatic in 13% of cases according to Langdown et al.1
The exact physiopathology of perineural cyst remains unclear, and several hypotheses have been proposed. Tarlov suggested that hemosiderin deposition caused blockage of the venous drainage of the perineurium and epineurium after local trauma can lead to the development of these cysts.4 Others authors discuss a developmental or congenital origin.8
The onset of symptoms can be sudden or gradual, and are exacerbated by coughing, standing, and change of position,8 those symptoms depend on their location, and range from backache, perineal pain or sciatica to over cauda equina syndrome.5
TC is usually diagnosed using diagnostic imaging. X-ray can show bone erosion in the anterior or posterior part of the vertebral foramen.9 The CT scan may show CSF isodense cystic mass at the foramen.10 Myelography was used for the positive diagnosis of TC, it allowed the identification of the communication of the cyst with the subarachnoid space, and late filling phenomenon allowing the differential diagnosis with other cystic lesions of meningeal origin, which are not TC.11
Spinal MRI is currently the method of choice in diagnosis of perineural cysts, it shows a cystic lesion, located near the dorsal root ganglion with a hypointense signal through T1-weighted imaging, a hyperintense signal through-T2 weighted imaging, without godalinium enhancement.
The differential diagnosis is mainly with other spinal meningeal cysts. The classification of Nabor et al.12 differentiates three types; Type I: extradural cysts without nerve fiber, type Ia: arachnoid cyst extradural. Type Ib: meningocele sacred. Type II: extradural cysts containing nerve cells (TC). Type III: arachnoid cyst intradural.12
It is also important to distinguish with neurogenic tumors such as schwannoma, those solid tumors enhance after gadolinium injection, Joshi et al. reported about a central perineural cyst masquerading a tumor, the cyst was located intra spinally and caused compression of the cervical myelon.13
Till date, published treatment options for apparently symptomatic TC include medication, percutaneous procedures, and surgery. However, these methods are associated with various outcomes and complications. Mitra et al.14 described a conservative approach for a symptomatic cervical TC using oral steroids after initial ineffective course of NSAIDs. A six-day-course of oral steroids was given, leading to relief of symptoms, as far as, the upper extremity motor strength was concerned, but with a slight increase in the patient’s sense of pain.14
Kim et al.15 performed a more invasive transforaminal epidural steroid injection for a case of symptomatic perineural cyst in the cervical spine.15 Epidural steroid injection was primarily employed to reduce neural inflammation causing radicular symptoms, but the follow-up MRI revealed a shrunken cyst in this case, which was an unexpected result of the intervention.
Jungwon Lee et al.16 Performed ultrasound-guided cervical elective nerve root block using local anesthetics and steroids without fenestration of the cyst in a case of symptomatic cervical TC which was resistant to medication.16 Therefore, ultrasound-guided cervical selective nerve root block is a safe and effective procedural option for the treatment of symptomatic cervical perineural cysts.
The microsurgical approach usually involves a small laminectomy with cyst fenestration, cyst imbrication, cyst neck ligation, cyst resection, and combinations of the above.8,17,18 Combining the evidence from 31 case series Laura E. Dowsett et al.19 found that after surgical treatment, the symptoms attributed to TC either completely or partially relieved in 83% of the cases. Complete resolution was experienced in 32% of cases, 50% had partial resolution, 16% had no improvement or worsening of symptoms and 0.4% had worsening of symptoms after surgery.19
However, the optimal management of symptomatic TC is still a matter of ongoing debate because of the variety of outcomes and complications for each method. Percutaneous aspiration of a perineural cyst can cause headaches owing to intracranial hypotension.2 Fibrin glue placement of perineural cysts is associated with several complications including aseptic meningitis and CSF leakage.20,21 Surgical excision of these cysts can also result in complications involving neural damage, pseudomeningocele, and intracranial hypotension.19
In conclusion, symptomatic cervical perineural cysts are extremely rare. In our patient’s previous report, because of the rarity of the lesion, we did not suspect a TC at first, however, it should kept in mind in front of any intraspinal cystic lesion, and surgical excision may be an effective option for symptomatic cases.
The authors declare that they have no competing interests.
There was no funding applicable for this case report.
MH wrote the case report and provided data according to CARE guideline and provided the figures, KC collected the patient data and obtained the informed consent, FL co-wrote and reviewed this case report, MH and KC operated the patient, MB and MFC did the final revision of this case report. All authors reviewed the final manuscript. All authors read and approved the final manuscript.
None.

©2019 Hammoud, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.