Journal of
eISSN: 2373-6410


Case Report Volume 14 Issue 2
Department of Neurosurgery, National Hospital of Niamey, Niamey, Niger
Correspondence: Ousmane Issoufou Hamma, Department of Neurosurgery, National Hospital of Niamey, Niamey, Niger
Received: March 20, 2024 | Published: April 5, 2024
Citation: Hamma OI, Daouda DH, Mato SS, et al. Ischemic stroke of posterior cerebral artery territories in a child after large traumatic subacute epidural hematoma: about a rare case report and literature review. J Neurol Stroke. 2024;14(2):41-42. DOI: 10.15406/jnsk.2024.14.00580
An epidural hematoma is a collection of blood in the epidural space and can occur after even minor head trauma. It is defined as the excellence of neurosurgical emergencies. In children, it is the most common posttraumatic intracranial hematoma, and is generally caused by falls from height or domestic accidents. However, in children, the increase in intracranial pressure is compensated for longer, due to the high compliance of the skull vault and brain parenchyma, but can suddenly lead to encephalic involvement and, in rare cases, even hemispheric infarction. Here, we report the case of a 23-month-old boy who presented with a subacute posttraumatic epidural hematoma complicated by cerebral infarction following a fall from a height. He was referred to us with an admission delay of 50 hours and was then rapidly taken to the operating room for emergency surgery. Unfortunately, the postoperative course was marked by complications. This case highlights that infarction during subacute epidural hematoma is a sign of a very poor prognosis.
Keywords: epidural hematoma, cerebral infarction, traumatic brain injury, head injury, children
CT, computed tomography; GCS, glasgow coma scale; EDH, epidural hematoma
Epidural hematoma is characterized by a collection of blood in the epidural space and is considered a major neurosurgical emergency.1,2 It is one of the most common subtypes of intracranial hematoma in children under four years of age, making it a genuine public health problem. In the pediatric population, it generally occurs following trauma from falls from height or domestic accidents.1,3–5 However, in children under the age of two, the increase in intracranial pressure is compensated for longer, due to the high compliance of the skull vault and brain parenchyma, but can suddenly lead to encephalic involvement.3 Nevertheless, in rare cases, the mass effect can also be complicated by parenchymal ischemia, particularly in the territory of the posterior cerebral artery.6–8 Here, we report the case of a patient with a subacute hematoma complicated by hemispheric infarction who was treated in our neurosurgery department and whose postoperative course was complicated.
The patient was 23 months old and was a victim of a fall from bed height with cephalic landing, resulting in a brief loss of consciousness and a return to a conscious state. Slight left parietal swelling developed in the hours following the trauma, prompting the parents to bring him from a local peripheral health center, where he was cared for and monitored for approximately 24 hours. He had started convulsing during the monitoring, which prompted his transfer to our center for further treatment, some 300 km away. It should be noted that his state of health deteriorated during his transfer to our center, with the onset of an intracranial hypertension syndrome characterized by worsening consciousness and vomiting.
At the hospital, the patient obnubilated with pediatric Glasgow Coma Scale (GCS) score of 12/15 (E3V4M5) and psychomotor agitation. His spontaneous movements were asymmetric, and his pupils were unequal in size and rapidly reactive to light. He had hemodynamic instability and pallor. Uninjected CT images (Figure 1) revealed a left parietal fracture, a subgaleal hematoma, a large left occipoparietal epidural hematoma with an infarct in the territory of the left posterior cerebral artery and midline deviation. Biological tests revealed anemia, with haematocrit decreasing to 5.12 g/dl. We diagnosed a hemispheric infarction in the territory of the posterior cerebral artery following a subacute epidural hematoma complicated by hemodynamic shock.
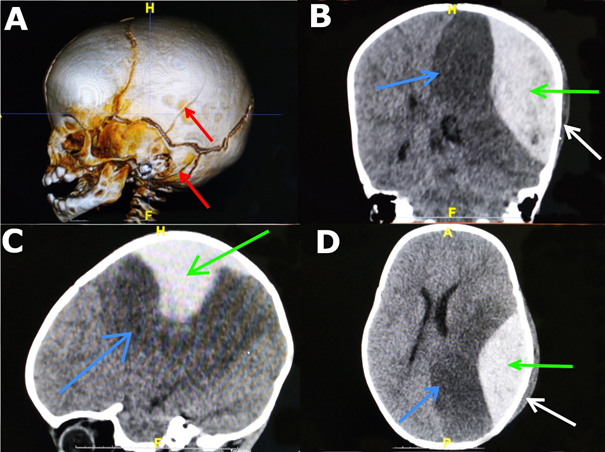
Figure 1 CT images of the patient showing: (A) 3D reconstruction of the temporoparietal fractures (red arrows); (B,C,D) parenchymal windows, the epidural hematoma (green arrow), the infarct in the territory of the left posterior cerebral artery (blue arrow) and the subgaleal hematoma (white arrow).
He was rapidly taken to the operating room, where a large cranial flap was performed, followed by evacuation of the hematoma and suspension of the dura mater. He had experienced several cardiac arrests during the surgery. He was taken directly to the intensive care unit after surgery. The immediate postoperative course was marked by hemodynamic instability, followed by death 48 hours after surgery despite intensive resuscitation.
Traumatic brain injuries remain the leading cause of death and disability in children and young adults.4 Fortunately, even patients with massive epidural hematomas evolve favorably when treated early and with good quality care. In infants, a massive epidural hematoma leads to intracranial hypertension, which is compensated for longer than in adults due to the large conformation of the cranial vault and brain, but can suddenly lead to a mesencephalic compression syndrome. This intracranial hypertension may progress to perioperative ischemic complications, the association of which with intracranial hematoma has been linked to an increased risk of death; however few cases have been reported in the literature.6–8 Nevertheless, there have been a few cases of ischemia following evacuation of an epidural hematoma, most of which had a favorable outcome.3 According to Ulrich et al, the cause of infarction in the territories of the middle and posterior cerebral vessels is linked to the vulnerability of cerebral vessels in children. While the elasticity of arterial walls during childhood is greater in older people, the walls are thinner and more tortuous than in adults due to the lack of collagen fibers. Compression of the posterior cerebral artery at the tentorial margin, resulting in infarction of the associated vascular territory due to intracranial mass lesions caused by displacement into the tentorial notch, is well described in the neuropediatric literature.3 Posttraumatic delayed epidural hematoma is a rare complication, but well described in the literature. The most widely supported hypothesis as to the mechanism responsible for the formation of a delayed posttraumatic epidural hematoma concerns above all the loss of a tamponade effect caused by the reduction of intracranial pressure with medical or surgical treatment. The second hypothesis is the rupture of a bridging vein close to a Pacchioni granulation, which leads secondarily to hematoma.3,9 In our patient, perioperative vascular shock can be explained by the sudden decrease in hemoglobin concentration due to massive epidural and subgaleal extravasations.3,5,9 According to Gutierrez et al, hemoglobin concentrations below 7 to 8 g/dl in the pediatric population aggravate hemodynamic instability, which can lead sequentially to decreased oxygen supply, reduced tissue perfusion, cellular hypoxia and organ damage.10 In our study, this hemodynamic instability exacerbated the hypoxic effects of hemispheric infarction, which likely led to the patient's death. It is therefore important to note that the development of hemispheric infarction and hypotension during the course of an epidural hematoma is a very poor prognostic factor.
Epidural hematoma is a potentially fatal complication of pediatric head trauma. Timely intervention and diagnosis reduce mortality and morbidity in many patients. However, the combination of hemispheric infarction and hemodynamic shock worsens the prognosis.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Consent was obtained from the patient's parents for writing the manuscript.
The study has been approved by the Ethics Committee of the National Hospital of Niamey.
All the authors have no conflicts of interest to declare.

©2024 Hamma, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.