eISSN: 2377-4304


Research Article Volume 13 Issue 2
1Obstetrics and Gynecology Department, Lebanese University, Beirut, Lebanon
2Obstetrics and Gynecology Department, Al Zahraa Hospital University Medical Center, Beirut, Lebanon
3Obstetrics and Gynecology Department, Makassed General Hospital, Beirut, Lebanon
4Head of Obstetrics and Gynecology Department, Al Zahraa Hospital University Medical Center, Beirut, Lebanon
5Head of Obstetrics and Gynecology Department Rafik Hariri Hospital University Medical Center, Beirut, Lebanon
6Assistant Professor Obstetrics and Gynecology Department Lebanese American University,Beirut, Lebanon
Correspondence: Dr. Kariman Ghazal, Obstetrics and Gynecology Department, Lebanese University, Beirut, Lebanon
Received: March 31, 2022 | Published: April 22, 2022
Citation: DOI: 10.15406/ogij.2022.13.00637
Objective: The goal of this study was to examine the clinical and ultrasonographic features of females who presented with abdominal discomfort and had ovarian torsion against those who did not.
Methods: This was a cohort study that looked back included all female patients who presented to a referral private clinic with pelvic and/or abdominal pain between January 2017 and December 2020. Patients who were clinically diagnosed with torsion but had negative intra-operative findings were excluded. Patients who met the criteria were separated into two groups (ovarian torsion vs. no torsion).Symptoms including the type, location and duration of pain, presence of nausea and vomiting, abdominal tenderness, presence of adnexal masses at digital examination, ultrasound findings, pre-operative diagnosis, final diagnosis, as well as surgical management were recorded.
Results: During the research period, a total of 65 female patients came with abdominal discomfort, with 17 (26.2%) having ovarian torsion and 48 (73.8%) not having torsion. 1 (5.9%) of the 17 patients with torsion were in their teenage years, 14 (87.4%) were in their reproductive years, and 2 (11.8%) were 51 years or older. All patients who had torsion presented with nausea and vomiting while none of the patients who did not have torsion had nausea and vomiting (p-value<0.0001). As for pain, 38 (79.2%) had moderate pain in the no torsion group compared to none in those who had torsion since all patients who had torsion had severe pain compared to 10 (20.8%) of those who did not have torsion (p-value<0.0001). Eight patients were pregnant, 5 without torsion and 3 with torsion. The length of discomfort in the torsion group was substantially longer than in the non-torsion group (52.6555.02 days vs. 16.3115.85, p-value0.0001, respectively). Three patients were menopausal, 1 with no torsion and 2 had torsion. Around 58% of the patients without torsion had negative Doppler findings for simple cyst compared to 23.5% of those with torsion. All patients who had torsion underwent surgery and all patients without torsion had regression of pelvic mass. For those who had torsion, 35.3% had their ovary removed, 58.8% had the cyst removed while ovary conserved, and 5.9% had drainage for the cyst.
Conclusion: Using a combination of presenting symptoms and ultrasonography, ovarian masses may be identified and ovarian torsion suspected. Torsion must be detected early in order to get conservative therapy and maintain the reproductive capacity of younger girls.
Keywords: ovarian torsion, abdominal pain, ultrasound
Ovarian torsion could occur in females of all ages but is most common in postmenarchal women.1 Torsion is caused by the twisting of the ovary on its pedicle, leading to obstruction of venous outflow, edema of the ovary and vascular pedicle, and restricted blood supply. This might result in ischemia, necrosis, and loss of function.2 The ovary, fallopian tube, or both are involved in adnexal torsion.3 More than 60% of instances of adnexal torsion have been observed to have concurrent ovarian and tubal torsion.3
The existence of an ovarian cyst or tumor, which twists the ovary along the utero-ovarian ligaments, is the most prevalent cause of ovarian torsion.3 The ovarian lump or cyst is almost always a benign tumor rather than a malignant one.4 Ovarian torsion can also happen during pregnancy. The risk is greatest in pregnant women between the ages of 10 and 17weeks of gestation, especially if they have an ovarian mass.5
The majority of people who have ovarian torsion have non-specific lower abdomen and pelvic discomfort, which can be intermittent or persistent.6 Patients may have occasional discomfort as a result of spontaneous torsion and detorsion.7 The level of discomfort varies. It isn't always as serious as it appears. Pain episodes might last for several days or even months before being diagnosed.6 Diffuse discomfort rather as concentrated lower abdomen pain is more common in premenarchal females.1 Nausea, vomiting, and a low-grade temperature are some of the other symptoms.
For ovarian torsion, ultrasound is the first imaging modality of choice. Torsion is characterized by an enlarged ovary as a result of venous or lymphatic engorgement, edema, and bleeding. Other symptoms include free pelvic fluid, an underlying ovarian lesion, a lack of vascularity, and a twisted vascular pedicle. The most frequent kind of ovarian torsion is unilateral.3 Ovarian torsion color Doppler imaging varies depending on the degree of vascular impairment. The lack of arterial flow is a typical color Doppler observation.3 Despite this, ovarian enlargement has been recorded as a torsion sonographic result, even in the presence of arterial and venous Doppler flow. If there are symptoms and the ovary is enlarged, ovarian torsion should be suspected, regardless of whether an ovarian Doppler result is present or not.8 If ultrasound findings are inconclusive, computed tomography (CT) may be used to aid in diagnosis.3
Because it is typical to overlook ovarian torsion in the differential diagnosis, despite its rarity, early detection is critical to avoid necrosis and maintain ovary viability. The goal of this study was to examine clinical and ultrasonographic features of females who presented with abdominal discomfort and had ovarian torsion against those who did not.
This was a cohort study that looked back that included all female patients who presented to a referral private clinic with pelvic and/or abdominal pain between January 2017 and December 2020. Patients who were clinically diagnosed with torsion but had negative intra-operative findings were excluded. Patients were identified from the medical record database. Patients who met the criteria were separated into two groups (ovarian torsion vs. no torsion). Surgical confirmation of ovarian torsion was obtained. The demographic information of the patients was gathered. Symptoms such as pain kind, location, and duration, nausea and vomiting, abdominal soreness, the presence of adnexal masses on digital examination, ultrasound findings, pre-operative diagnosis, final diagnosis, and surgical care were all documented. Transverse and longitudinal ultrasound images of the uterus and ovaries were taken utilizing a transabdominal and intravaginal technique. Doppler flow measurements in the vessels were taken. The uterus, ovaries, and any adnexal lumps were all measured and documented.
For the study, the Statistical Package for Social Sciences (SPSS, version 24) application was utilized. Continuous variables were reported as mean and standard deviation, whilst categorical variables were provided as number and percent. For comparing categorical variables, bivariate analysis was performed using the Chi square test or Fisher's exact test (where appropriate). The Student's t-test was used to compare continuous variables. The statistical significance was determined using a p-value of less than 0.05.
During the research period, A total of 65 female patients presented with abdominal pain during the study period, of which 17 (26.2%) had ovarian torsion and 48 (73.8%) did not have torsion. Of the 17 patients who had torsion, 1 (5.9%) was in the adolescent age group, 14 (87.4%) were in the reproductive age group, and 2 (11.8%) were 51 years or older. The demographic characteristics of patients in the two groups were similar (Table 1).
Variable |
No torsion (n=48) |
Torsion (n=17) |
p-value |
|
Age |
Years |
34.92±10.99 |
34.47±14.04 |
0.89 |
Age category |
14-19 years (adolescent) |
4 (8.5%) |
1 (5.9%) |
0.75 |
20-50 years (reproductive age) |
40 (85.1%) |
14 (82.4%) |
||
≥51 years |
3 (6.4%) |
2 (11.8%) |
||
BMI |
Normal |
5 (10.4%) |
1 (95.9%) |
0.42 |
Over-weight |
14 (29.2%) |
7 (41.2%) |
||
Obese |
29 (60.4%) |
9 (52.9%) |
||
Education |
Middle school |
4 (8.3%) |
1 (5.9%) |
0.9 |
High school |
24 (50.0%) |
8 (47.1%) |
||
University |
20 (41.7%) |
8 (47.1%) |
||
Employment |
13 (27.1%) |
2 (11.8%) |
0.32 |
|
Residency |
Urban |
6 (12.5%) |
1 (5.9%) |
0.67 |
|
Rural |
42 (87.5%) |
16 (94.1%) |
|
Table 1 Patients’ demographic characteristics
All patients who had torsion presented with nausea and vomiting while none of the patients who did not have torsion had nausea and vomiting (p-value<0.0001). As for pain, 38 (79.2%) had moderate pain in the no torsion group compared to none in those who had torsion since all patients who had torsion had severe pain compared to 10 (20.8%) of those who did not have torsion (p-value<0.0001). Around 91% of the patients who did not have torsion had their pain before cycle compared to 40% of those who had torsion, whereas none had pain after the cycle in the no torsion group compared to 30% of the torsion group. Eight patients were pregnant, 5 without torsion and 3 with torsion, each had pain in a different trimester. Eight patients, five without torsion and three with torsion, were pregnant and each felt discomfort in a different trimester. Diffuse abdominal discomfort was reported by 39 percent of individuals without torsion and 70.6 percent of those with torsion. Around 39% of patients without torsion had diffuse abdominal pain compared to 70.6% of those who had torsion. Right lower quadrant pain was present in 41.7% of patients with no torsion compared to 23.5% of torsion patients. Four patients (8.3%) who did not have torsion had low back pain compared to none in those with torsion. The length of discomfort in the torsion group was substantially longer than in the non-torsion group (52.6555.02 days vs. 16.3115.85, p-value0.0001, respectively. Other symptoms were amenorrhea (60.4% vs 41.2% in the no torsion vs. torsion groups respectively) and irregular bleeding (27.1% vs. 29.4% in the no torsion vs. torsion groups respectively). Three patients were menopausal, 1 with no torsion and 2 had torsion (Table 2).
Variable |
|
No torsion (n=48) |
Torsion (n=17) |
p-value |
Nausea and vomiting |
0 (0.0%) |
11 (64.7%) |
<0.0001 |
|
Pain |
Moderate |
38 (79.2%) |
0 (0.0%) |
<0.0001 |
Severe |
10 (20.8%) |
17 (100.0%) |
||
Pain timing |
Before cycle |
43 (91.5%) |
4 (40.0%) |
0.006 |
After cycle |
0 (0.0%) |
3 (30.0%) |
||
First trimester |
5 (10.4%) |
1 (10.0%) |
||
Second trimester |
0 (0.0%) |
1 (10.0%) |
||
Third trimester |
0 (0.0%) |
1 (10.0%) |
||
Site of pain |
Diffuse abdominal pain |
19 (39.6%) |
12 (70.6%) |
0.04 |
Right lower quadrant |
20 (41.7%) |
4 (23.5%) |
||
Left lower quadrant |
5 (10.4%) |
1 (5.9%) |
||
Low back pain |
4 (8.3%) |
0 (0.0%) |
||
Duration of pain |
Days |
<0.0001 |
||
Symptoms |
Amenorrhea |
29 (60.4%) |
7 (41.2%) |
0.07 |
Irregular bleeding |
13 (27.1%) |
5 (29.4%) |
||
Pregnant |
5 (10.4%) |
3 (17.6%) |
||
Menopause |
1 (2.1%) |
2 (11.8%) |
||
Ultrasound images |
Liquid content |
38 (79.2%) |
4 (23.5%) |
0.003 |
Solid content |
0 (0.0%) |
1 (5.9%) |
||
Complex cyst |
7 (14.6%) |
12 (70.6%) |
||
Liquid multiseptum cyst |
2 (4.2%) |
0 (0.0%) |
||
Solid multiseptum cyst |
1 (2.1%) |
0 (0.0%) |
||
28 (58.3%) |
4 (23.5%) |
0.05 |
||
Solid Doppler negative |
0 (0.0%) |
1 (5.9%) |
||
Complex cyst Doppler negative |
2 (4.2%) |
1 (5.9%) |
||
Complex cyst Doppler positive |
2 (4.2%) |
7 (41.2%) |
||
Liquid multiseptum cyst Doppler negative |
10 (20.8%) |
0 (0.0%) |
||
Solid multiseptum cyst Doppler negative |
1 (2.1%) |
1 (5.9%) |
||
Pregnant simple cyst Doppler negative |
4 (8.3%) |
0 (0.0%) |
||
Pregnant complex cyst Doppler negative |
1 (2.1%) |
1 (5.9%) |
||
Pregnant complex cyst Doppler positive |
0 (0.0%) |
2 (11.8%) |
||
WBC |
≤10 |
47 (97.9%) |
5 (29.4%) |
<0.0001 |
>10 |
1 (2.1%) |
12 (70.6%) |
||
Underwent operation |
0 (0.0%) |
17 (100.0%) |
<0.0001 |
|
Regression of cyst |
48 (100.0%) |
0 (0.0%) |
<0.0001 |
|
Treatment |
Analgesics |
16 (33.3%) |
12 (70.6%) |
0.18 |
Progesterone |
30 (62.5%) |
2 (11.8%) |
||
|
Analgesics and progesterone |
2 (4.2%) |
3 (17.6%) |
|
Table 2 Clinical and ultrasonographic characteristics of patients
Ultrasound done at presentation showed that 79.2% of patients without torsion had liquid content in comparison to 23.5% in those with torsion. A single patient with torsion had solid cyst content and the majority had complex cyst. Around 58% of the patients without torsion had negative Doppler findings for simple cyst compared to 23.5% of those with torsion. Doppler findings were positive for complex cyst in 41.2% of patients with torsion versus 4.2% of patients without torsion. More patients without torsion had negative Doppler findings for liquid multiseptum cyst while negative Doppler findings were similar in both groups for solid multiseptum cyst. As for the five pregnant patients without torsion, four patients had negative Doppler findings for simple cysts and one patient had negative Doppler for complex cyst. Of the three pregnant patients who had torsion one patient had negative Doppler and two had positive Doppler for complex cyst (Table 2).
White blood cell counts were found to be higher in the torsion group (p-value 0.0001) in laboratory investigations. All patients who had torsion underwent surgery and all patients without torsion had regression of pelvic mass. Around 33% of patients without torsion consumed analgesics compared to 70% of patients with torsion while more patients in the no torsion group (62.5%) took progesterone (Table 2).
For those who had torsion, 35.3% had their ovary removed, 58.8% had the cyst removed while ovary conserved, and 5.9% had drainage. Causes of torsion were: 17.6% hemorrhagic cyst, 29.4% hemorrhagic cyst and ovary necrosis, 17.6% serous cystadenoma, 5.9% necrotic ovary, 5.9% para-ovarian cyst, 17.6% teratoma, and 5.9% abscess from rectal cancer (Table 3).
Variable |
|
Number (%) |
Operation type |
Remove ovary |
6 (35.3%) |
Remove cyst and keep ovary |
10 (58.8%) |
|
Drainage |
1 (5.9%) |
|
Torsion reason |
Hemorrhagic cyst |
3 (17.6%) |
Hemorrhagic cyst and ovary necrosis |
5 (29.4%) |
|
Serous cystadenoma |
3 (17.6%) |
|
Serous cystadenoma and ovary necrosis |
1 (5.9%) |
|
Teratoma ovary necrosis |
3 (17.6%) |
|
Para-ovarian cyst |
1 (5.9%) |
|
|
Abscess from rectal cancer |
1 (5.9%) |
Table 3 Operative outcome of patients with ovarian torsion
Case 1: A 67-year-old lady (gravida 5, para 3, abortions 2) complained of nausea and lower right abdomen discomfort. The lower abdomen was soft on physical examination, with minor soreness in the right adnexa. Ultrasound examination revealed a slightly enlarged right ovary with normal appearance and Doppler imaging showed inside flow with echogenic side and presence of echogenic cyst. Torsion of the right adnexa with ovarian cyst was discovered during a laparotomy. Hysterectomy and bilateral salpingectomy were done (Figure 1). Histology results were torted ovarian serous cystadenoma with atrophic endometrium.
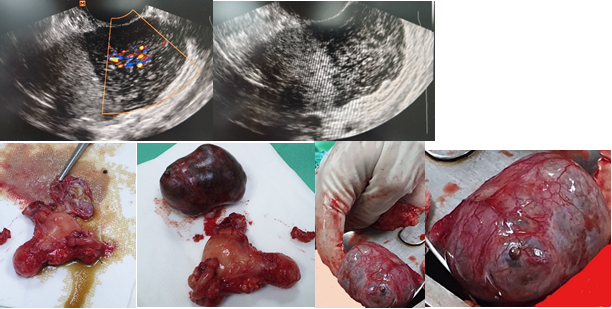
Figure 1 Vaginal ultrasound pictures demonstrating a big ovary (> 4 cm) with edema and a positive intra-ovary Doppler. An ovarian serous cystadenoma with atrophic endometrium was discovered during surgery.
Case 2: A 45-year-old lady (gravida 5, para 3, abortions 2) complained of acute lower right abdomen discomfort, nausea, and walking trouble. The lower abdomen was soft on physical examination, with minor soreness in the right adnexa. An enlarged right ovary edema was discovered on ultrasound, and Doppler imaging demonstrated flow in the wall and negative center, as well as adnexal torsion consistent with simple ovarian cysts. The ovary on the opposite side was normal. The torn ovary was swollen, edematous, and lacked definition. Torsion of the right adnexa with ovarian cyst was discovered during a laparotomy. The procedure included a hysterectomy and bilateral salpingectomy (Figure 2). Endometrial hyperplasia with torted ovary was discovered on histology after operation.
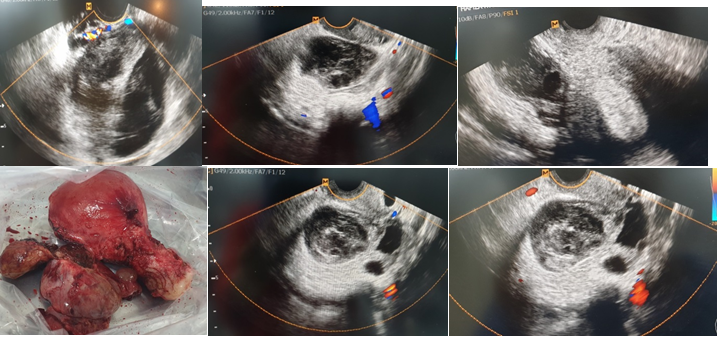
Figure 2 Ultrasound pictures of the pelvis and vaginal canals reveal massive, heavy cysts on the periphery (the string of pearls sign). The cysts are unilateral in ovarian torsion and have aberrant ovary morphology (congested ovarian stroma). A clockwise or counterclockwise wrapping of hypoechoic vessels around the central axis is apparent as the "whirlpool" sign.
Case 3: A 26-year-old patient presented with severe pain, nausea and vomiting, and amenorrhea. Her pregnancy test was positive. Pelvic ultrasound showed right ovarian cyst fluid with septum negative Doppler at 7 weeks (Figure 3). She was given treatment with progesterone for 4 weeks. She had regression of the cyst after 11 weeks.
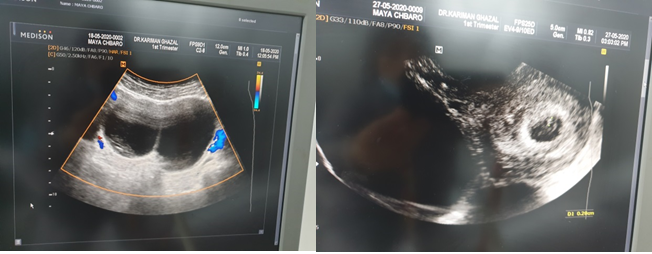
Figure 3 Pelvic ultrasound showing ovarian cyst >5cm with septum negative Doppler and gestational sac at 7 weeks.
Case 4: A 17-year-old girl came to the hospital with acute lower right abdomen discomfort, nausea, trouble walking, and irregular menstruation. The lower abdomen was not soft on physical examination, and the right adnexa were somewhat painful. An enlarged, hemorrhagic, torted right ovary was seen on ultrasound, with Doppler imaging revealing outer flow with a negative core. Torsion of the right adnexa with teratoma was discovered during a laparotomy. Hemostasis was performed after the teratoma was excised (Figure 4). The diagnosis was confirmed by histology.
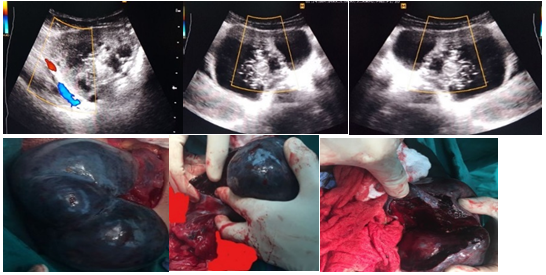
Figure 4 Large, hefty cysts and immature cystic teratomas that are benign. With solid component, peripheral cysts (the string of pearls sign) might be visible; the cysts are unilateral in ovarian torsion with aberrant ovary shape.
Case 5: A 27-year-old woman complained of acute lower right abdomen discomfort, nausea, and vomiting, as well as difficulties walking and irregular menstruation. The lower abdomen was not soft on physical examination, and the left mass was slightly painful. An increased pelvic mass edema was seen on ultrasound, and Doppler imaging demonstrated flow in the wall with a negative intra-cyst. The right ovary had a solid mass of 6 cm, while the left ovary had a solid mass of 3 cm. Torsion of the paraovarian mass with teratoma and hemorrhagic cyst were discovered during laparotomy. Hemostasis was performed after the teratoma and hemorrhagic cyst were excised (Figure 5). The diagnosis was confirmed by histology.
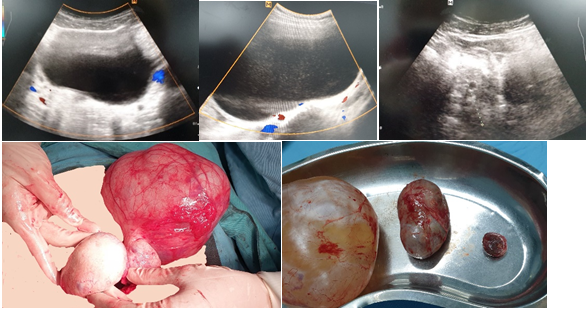
Figure 5 Torted paraovarian mass with large, heavy cystic neoplasms with negative Doppler and unknown substance.
Case 6: A 39-year-old woman (gravida 2, para 2) appeared with significant lower right stomach discomfort, nausea, and trouble walking after being on contraceptive tablets for several years. Thelower abdomen was not soft on physical examination, and the right mass was slightly painful. An increased right mass edema was discovered on ultrasound, and Doppler imaging flow was positive in the wall but negative within. The ovary was saved after a laparotomy revealed a benign cyst adenoma that was excised (Figure 6).
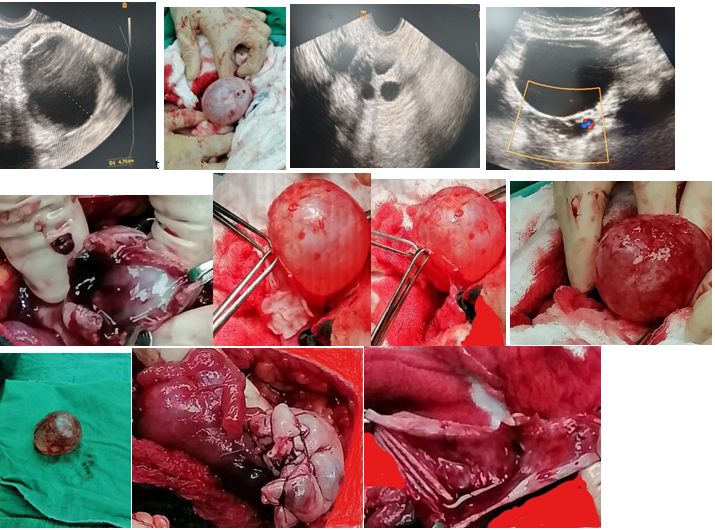
Figure 6 Ultrasound scans of the pelvis and vaginal canals demonstrating peripheral cysts (the string of pearls sign). Torted ovary with large, massive unilateral cyst and aberrant ovarian morphology.
Case 7: Severe discomfort and irregular menstruation plagued a 48-year-old woman. Ultrasound indicated the proper bulk, which had both liquid and solid material (8cm). The ovary was removed after a laparotomy discovered a cyst adenoma (Figure 7).
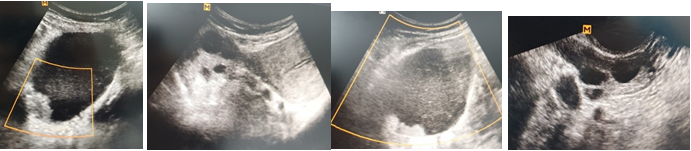
Figure 7 Ultrasound imaging of the right mass, which contains both liquid and solid material. The ovary on the opposite side is typical, having a multifollicular appearance.
Case 8: The patient, a 39-year-old woman, was in excruciating agony and vomiting. Ultrasound of the pelvis and vaginal cavity revealed a complicated mass (>5cm). Doppler showed a negative result. A laparotomy revealed a hemorrhagic cyst in torsion (Figure 8). The diagnosis was confirmed by histology.

Figure 8 Ultrasound of the pelvis and vaginal region revealed a complicated mass with a solid component papillary appearance and a negative result. Doppler.
Case 9: Severe discomfort, nausea, and amenorrhea were reported by a 16-year-old patient. Ultrasound of the pelvis revealed a complicated mass with liquid and solid material. Doppler showed a negative result. She took analgesics and had relapse following the cycle (Figure 9).
Case 10: A 34-year-old woman (gravida 2, para 2) arrived with significant lower right abdomen discomfort, nausea, and walking trouble. The lower abdomen was not soft on physical examination, and the right mass was slightly painful. An enlarged right mass was discovered during a pelvic and vaginal ultrasound examination. The flow was positive in the wall but negative inside, according to Doppler imaging. The torsion of a benign serous cystadenoma was discovered during a laparotomy, and it was excised while the ovary was preserved (Figure 10).
The study's primary finding was that 26.2 percent of female patients with abdominal discomfort also had ovarian torsion. Those had severe pain as well as nausea and vomiting. All underwent surgery and more than half of them (58.8%) had their ovaries conserved.
Ovarian torsion occurs when the ovarian vascular pedicle rotates partially or completely, obstructing arterial and venous input and outflow3 Though it is most common in the reproductive age group, it is reported in both prepubertal girls and postmenopausal women.4,9 According to Ashwal et al, 16% of cases were premenarchal and 83% were postmenarchal.1 Another study reported that 66.7% of ovarian torsion cases were in the reproductive age and 11% of the patients were postmenopausal patients.9
In this study, ovarian torsion was seen in one patient 1(5.9%) in adolescent group, 14 patients (82.4%) in the reproductive age group and 2 patients (11.8%) in the menopausal group.
At the time of presentation, adnexal torsion presents a variety of indications and symptoms. The most common symptom is abdominal pain, which is followed by nausea and vomiting Abdominal discomfort is the most prevalent symptom, followed by nausea and vomiting.10 Continuous dull pain was the most prevalent symptom in postmenopausal patients (57%), while acute-onset sharp pain was the most common symptom in premenopausal women, according to Cohen et al (86%).11 Pain is generally intermittent and appears suddenly.10 Pain episodes might last for several days, weeks, or even months.6,12 Previous partial torsion6 or spontaneous detorsion7 may cause similar temporary pain episodes. All of the participants in this research experienced abdominal discomfort. All patients with torsion experienced severe pain, however for the most part, the discomfort was sporadic. The majority of individuals who did not have torsion reported discomfort prior to the cycle, whereas those who did had torsion had pain after the cycle. Torsion patients had discomfort for an average of 52 days on average. Right lower quadrant discomfort affected 23.5 % of torsion patients, compared to 5.9% who had left lower quadrant pain and 70.6% t who had diffuse abdomen pain.11Torsion usually occurs unilaterally with around 58% of cases seen on the right side. This could be due to the protection of the left ovary by the sigmoid colon.1,3,9
Furthermore, ovarian torsion has been linked to the existence of ovarian masses greater than 5cm,13 showing that an ovarian mass is the major risk factor for ovarian torsion.10 The majority of individuals with ovarian torsion in our research had ovarian masses ranging in size from 5cm to 20cm. In pregnancy, ovarian torsion has been found to occur in 10-14% of cases.5,14 The risk was increased between 10 and 17 weeks of pregnancy.
In terms of imaging, ultrasonography has been the most widely used tool for detecting ovarian torsion.6,10 The component, position, size, and Doppler flow of an ovarian tumor may all be determined by ultrasound.6,10 Absent venous Doppler flow is typical in ovarian torsion, according to certain studies,6 al beit it does not occur in every occurrence of torsion. Other research1,12 describes a whirlpool indication of twisted arteries visible with Doppler flow. In the current study, 7 (41.1%) of torsion patients had negative Doppler, whereas 8 (47%) had positive Doppler
Surgical confirmation and treatment of torsion remain the gold standard, despite the use of imaging.10 Postmenopausal patients had more extensive surgery, such as bilateral salpingo-oophorectomy with or without complete abdominal hysterectomy, than premenopausal patients had more conservative surgery (detorsion).6,10,15,16 In this research, 58.8% underwent conservative surgery and 35.3 percent had ovary removal, with two cases requiring hysterectomy. Because she had adhesions in the colon and abdominal wall, a single patient required abscess drainage for metastatic carcinoma.
Hemorrhagic cyst, teratoma, and serous cystadenoma are the most prevalent pathologic causes for torsion.14,15 According to Houry et al, 28.7% of patients had hemorrhagic cysts, 21.8 percent had benign teratomas, and 12.6 percent had serous cystadenomas.14 Balci et colleagues found 32% teratoma and 10.6% serous cystadenoma in their study.15 In our study, 8 (47%) of the cases with torsion on had hemorrhagic cysts, with 5 patients having ovarian necrosis, 4 (23.6%) having serous cystadenoma, and 3 (17.6%) having teratoma.
While diagnosing ovarian torsion might be difficult, a combination of presenting symptoms and ultrasonography can help locate ovarian masses and rule out ovarian torsion. Torsion must be detected early in order to get conservative therapy and maintain the reproductive capacity of younger girls.
None.
None.
Authors declare that there is no conflict of interest.

©2022 , et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.