eISSN: 2377-4304


Research Article Volume 12 Issue 6
1Hospital Aleman, Buenos Aires, Argentina
2Cleveland Clinic, Weston Florida, USA
3Surgery assistant, Hospital Aleman, Buenos Aires, Argentina
Correspondence: Alfredo Camargo, Gynecology Service, German hospital. Buenos Aires (CABA), Universidad de Buenos Aires, Argentina, Tel 5491154046953
Received: December 07, 2021 | Published: December 17, 2021
Citation: Bianchi F, Camargo A, Dip F, et al. Fluorescent sentinel lymph node mapping with icg in endometrial cancer. An initial experience in Argentina. Obstet Gynecol Int J. 2021;12(6):395-399. DOI: 10.15406/ogij.2021.12.00612
Background: Near-infrared fluorescence-based sentinel lymph node (SLN) mapping technique with indocyanine green (ICG) has been found a useful surgical modality for sentinel node detection and disease staging in endometrial cancer (EC) worldwide.
Objective: We aimed to introduce the SNL mapping technology using ICG and Near Infrared (NIR) fluorescence in Argentina. We aimed to assess the overall and bilateral detection rate of ICG based SNL mapping along with verifying its feasibility and effectiveness in surgical staging. We also aimed to discover the perceptions of surgeons regarding the use of ICG as a tracer and NIR as light-medium in SNL mapping.
Method: ICG SLNs identification was evaluated retrospectively. This study was performed at the Hospital Aleman de Buenos Aires in September, 2017The detection rates were calculated along with the analysis of the number of SNL observed and operative time, and time taken by overall surgery. Subsequently, the surgeons were interviewed to ascertain their opinion of using ICG SNL mapping in endometrial cancer staging.
Results: Four patients with endometrial cancer were included for analysis. The overall and bilateral detection rates have been 100% and 75%, respectively. While, under white light, no SLNs were identified. The average operative time of nodes resection was estimated 2.15 minutes. The fluorescence has been used for 2.2 minutes and overall time taken by surgery was estimated 71.5 minutes. The estimated blood loss (EBL) has been lower than 50 ml. The responses of surgeons’ from the interview have been 100% positive. The cost of the procedure based on the amount of dye used was 25 dollars per patient.
Conclusion: Laparoscopic ICG SLN resulted to be feasible, practical and no expensive surgical modality for uterine cancer triage.
Endometrial cancer (EC) is one of the most prevalent and increasing gynecological malignancy worldwide, especially in developed countries. Screening of lymph node metastases serves as a significant contributor to timely prognosis and delivers substantial oncologic information.1 The surgical approach for detecting the cancer stage in uterine cancers has been controversial, and it is suggested that conducting the pelvic or para-aortic lymphadenectomy for screening early-stage metastases can deliver adverse and unpropitious outcomes. Various approaches were introduced and evaluated for the same purpose that can impose minimal risk in any stage of EC.2–4
The intra-operative procedures in uterine cancer patients have been found very risky, but due to scarce knowledge and data, there was no other option except extensive lymphadenectomy which has been found to be associated with high morbidity. In recent years, the advancement of medical technology has led to the development of fluorescent sentinel lymph node (SLN) mapping in various tumor development sites.5 Earlier it has been successfully implemented in the screening of other tumors including malignant melanoma, breast cancer,6 bladder cancer7 and vulvar cancer. Due to its effectiveness and successful application, the fluorescent SLN approaches were proposed to be adopted for uterine cancer triage, especially EC and cervical cancer.8
The primary aim of this analysis was to evaluate the effectiveness of fluorescent technique of SLN mapping in EC staging using ICG dye in Argentina.
This study is conducted at Hospital Aleman de Buenos Aires in September 2017. Firstly, the four cancer patients were randomly selected between the age range of 55-87, for retrieving the clinicopathological data and oncologic information using proposed techniques. Physicians were interviewed, and their responses were collected to analyze the comfort of using the device.
A Storz SPIES Full HD D-Light P ICG technology (Karl Storz, Mittelstrasse, Tuttlingen, Germany) was used. Indocyanine green (Verdy) was used as a tracer, and NIR light was used to screen the SLNs.
To evaluate the applicability and effectiveness of ICG with NIR fluorescence based SLN mapping in oncology surgeries, different previous studies were analyzed.2,9–11
The solution with ICG was prepared with 25mg of ICG powder diluted into 10 ml of sterile aqueous water. Afterwards 2 ml of this solution was injected into cervix in two distinct positions, 3- and 9- o’clock positions. Half milliliter of ICG solution was administered with penetration to 1 cm deep into the stroma, and 0.5 mL was administered into the submucosal layer on both sides of the cervix. Subsequently, the NIR fluorescence was applied for SLN mapping, and the findings were recorded and analized (Table 1) (Table 2). The main variables that were determined for assessing the efficiency level of this technique in this series of research included time of migration of the dye, number of SLN detected with fluorescence in the pelvis, and the number of lymph vessels visualized. Moreover, we sought to evaluate the surgeons satisfaction, operative time and the time the fluorescent system was used.
|
Age |
Pathology |
SLNs |
SLNs |
SLNs |
ICG |
Site of |
Time of initialmigra-tion |
Time to |
Vessels |
Surgeon |
Opera-tive |
Total |
Overall |
|
66 |
Endometrial Adenocarcinoma |
0 |
0 |
2 |
5 mg |
3y9 O clockcervix |
3 min |
6 min |
3 |
8 |
1.3 min |
2.5. min |
55 min |
|
87 |
Endometrial Adenocarcinoma |
0 |
2 |
1 |
50 mg |
3y9 O clock cervix |
4 min |
6,30 min |
4 |
10 |
3.1 min |
2.7 min |
70 min |
|
55 |
Endometrial Adenocarcinoma |
0 |
1 |
1 |
5 mg |
3y9 O clockcervix |
5 min |
7,30 min |
2 |
10 |
2.2 min |
1.9 min |
68 min |
|
65 |
Endometrial Adenocarcinoma |
0 |
1 |
1 |
5 mg |
O clock3y9 cervix |
5 min |
6,50 min |
4 |
Not sure |
10 |
2.0 min |
93 min |
Table 1 Data gathered from the initial experiment of SNL mapping using ICG under NIR light in comparison of white light
|
Patients (N) |
4 |
|
Median age, years (range) |
65.5 (55-87) |
|
Mean age |
68.25 |
|
Patients with lymph node metastasis |
0% (0/4) |
|
Numbers of SLN detected on right side |
100% |
|
Numbers of SLN detected on left side |
75% (3/4) |
Table 2 Clinicopathologic characteristics of patients
After that, the four surgeons involved in this study were interviewed based on seven-questions regarding their experiences and findings of the technique (Table 3).
The findings from the applied technique showed the comparative results from the mapping (Figures 1–5).
The median age of the participants were 65.5 (55-87). When white light was used no SLNs were identified. When NIR light was used, SLNs were identified in all the patients (4/4), 100% and in 3 out of 4 patients bilateral nodes were detected 75% (Figure 6).
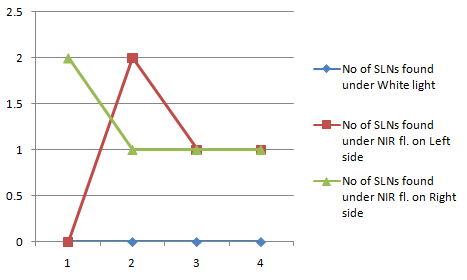
Figure 6 Chart showing a comparative graph for SLN detect under White light and NIR in left and right side (x axis-Patients & y axis-no. of SLNs).
The mean time of migration of ICG has been estimated as 4.25 minutes, and identification process of SLNs took an average of 6.52 minutes. Overall 13 lymph vessels were visualized in 4 patients. No metastasis was observed in detected SLNs. Mean surgeon satisfaction rate was 9.5 (95%). The mean operative time of nodes resection was estimated in 2.15 minutes.. The mean time of the use of fluorescence was 2.2 minutes. The overall surgical time was 71.5 minutes. The EBL (estimated blood loss) was less than 50 ml for each case. The cost of fluorescent SLN identification was 25 dollars per patient.
The interview responses delivered 100% positive responses from the surgeons (Table 3). The significant advantages of ICG based SLN mapping has been found fast, cost-effective and inexpensive.
|
Surgeons’ opinion |
Surgeon 1 |
Surgeon 2 |
Surgeon 3 |
Surgeon 4 |
|
Do you find the method useful? |
Yes |
Yes |
Yes |
Yes |
|
Do you believe it will become stándard of care (1 - 10)? |
10 |
10 |
10 |
10 |
|
Did you find it practical (1- 10)? |
10 |
10 |
10 |
10 |
|
Would you use it again? |
Yes |
Yes |
Yes |
Yes |
|
How frequently would you use it? (never, sometimes or always) |
Always |
Always |
Always |
Always |
|
Did the method guide you to the procedure? |
Yes |
Yes |
Yes |
Yes |
|
Did you find the method safe? |
Yes |
Yes |
Yes |
Yes |
Table 3 Data gathered from interviewing four surgeons’
All the patients were discharged two days after the procedure without any complications.
The present retrospective pilot study included four patients and delivered 100% and 75% overall and bilateral detection rates that are parallel to the results of Plante and Papadia’s work.2,4,12,13 The major points that are concluded by this research are that ICG serves an excellent and safe tracer for NIR fluorescence-based SLN mapping. It also delivers the highest overall and bilateral detection rate in comparison to other options, including blue dye, 99mTC (technetium-99m radiocolloid) and the use of white light.10 Previous studies have shown the potential of ICG as a tracer in NIR fluorescence in SLN mapping which is confirmed by the results of this retrospective study. Multiple studies have established the outstanding performance of ICG in SLN detection.2,3,9,10,11,14 The little variations are seen among the results from these studies which may be due to the various sample size chosen for the studies.
In this process, the cervical injection was filled with indocyanine-green (ICG) fluorescent dye followed by near-infrared fluorescence (NIR) imaging. It has delivered abundant outcomes in all type of surgeries including laparoscopic, open as well as robot-assisted surgery. It has been reported that ICG induced fluorescence in SLN mapping has been more productive and achieves higher total and bilateral pelvic SLNs detection-rates with reduced false negative rates and no side-effects.15,16
A UK based prospective study confirmed that SLN mapping might diminish surgical morbidity risk associated with lymphadenectomy. It discovered that SLN using ICG induced NIR fluorescence in open as well as laparoscopic surgeries delivered 100% optimization and detection rate for all type of cancers including uterine and vulvar.17 Buda and co-researchers9 conducted a comparative study with the aim of determining the detection rate and optimal bilateral mapping of SLNs using ICG, standard 99mTc and blue dye. This study concluded that SLN mapping using ICG delivers higher detection rate in comparison to other dyes. Furthermore, it has been shown superior performance in optimal bilateral mapping for early-stage cancer. The early prophylaxis through ICG based SLN mapping offers twofold advantages, firstly, it decreases the requirement of complete lymphadenectomies and secondly, it cuts the cost of the extensive surgical procedure and additional surgical expenses.9,18 This fact was further strengthened by the evidence provided by How et al.11 The authors highlighted the expediency and superior sensitivity of ICG dye in SLN mapping for para-aortic and pelvic areas.11 Papadia et al. showed a lower rate of false negative (FN) rate (8.3%) with almost 96% overall detection rate and 88% bilateral detection rates.2
The SLN mapping facilitates sensitive detection of lymph node metastases with the less comprehensive process and surgical trauma. The other significant advantage of SLN mapping approach is that it provides an effective staging procedure facilitating an appropriate triage of the patient for adjuvant therapies. SLN mapping technique is also associated with lower estimated blood loss and less operative time.2 It is suggested that SLN mapping approach has filled a significant gap between the extensive lymphadenectomy and no lymphadenectomy options in EC staging.3,19
The NIR fluorescent activation provides normal-colored anatomy expressions.4 The comparative analysis of imaging techniques for SLN mapping also confirmed that ICG as a tracer is the best modality superior to other options of colorimetric imaging20 or imaging under white light.10
We believe that the attained overall and bilateral detection rates in this study were contributed by the chosen tracer, ICG. Furthermore, in ICG based SLN mapping the risk of negative impact of BMI on detection is also diminished which is mainly faced with the other dyes like ISB (isosulfan blue).21,22 This finding was supported by Holloway et al.10 through a cohort study in which they showed the additional probability of improvement in detection accuracy from NIR technique. In this study, the authors emphasized that the detection rate of NIR fluorescence was further enhanced by adding ICG with ISB dye. The increased accuracy was evaluated in this case for detecting high numbers of SLNs and LN metastases in comparison of ISB alone. This combination produced higher detection rate and sensitivity without any risk of adverse outcome.10
In this retrospective pilot study, a small group of surgeons was interviewed, and their responses were gathered. Their experience and perceptions regarding the applicability of ICG in SLN mapping were assessed and compared for determining the values of defined variables. Their responses were similar to the predicted results from the other studies. The involved surgeons provided 100% feedback about its feasibility, detection rate and diagnostic accuracy in cancer patients. According to the literature most surgeons prefer to use dyes in SLN mapping in comparison of radioactive colloid due to the high potency, technical ease and cost-effectiveness.10 The surgeons found SLN mapping feasible and oncologically safe. The comparative evaluation of features, toxicity and clinical implications of 99mTC radiocolloid, blue dyes (including methylene blue, and isosulfan blue) and ICG revealed that ICG possesses an outstanding toxicity profile with higher overall as well as bilateral detection rates than blue dyes.23 Moreover, it has been shown superior detection rate with the NIR technology when compared to 99mTC and blue dye. ICG use as a tracer during mapping negates the impact of BMI on detection rates. Overall, SLN with ICG offers a cost-effective approach which is favored by surgeons as well as patients too.24,25
The weakness of this study is the small number of patients. Though, it has met all of its objectives and delivered the outcomes as expected.
The interview-based experiment also showed that the surgeons prefer this technique due to its nil toxicity, high detection rate and less extensive surgical procedure as well as less surgical trauma on patients. It has offered the best modality for SLN mapping in uterine malignancies. Its ease, no radiation exposure, cost-effectiveness, and quick procedures have led the surgeons to prefer it over other options.
This research showed that laparoscopic fluorescent SLN mapping using ICG is a feasible and cost effective surgical modality in oncologic staging, especially for endometrial cancer. SNL mapping in endometrial cancer with ICG plus NIR fluorescence is a valid option for staging purpose and it fills the gap between the choice of the complete lymphadenectomy or nothing, which had been found perilous for cancer patients. It will be highly valuable when 99mTC is not available because it will not only reduce the surgical cost, it will also provide appropriate and timely triage to the endometrial cancer patients in this country.
None.
None.
None of the authors has reported any conflicts of interest.

©2021 Bianchi, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.