eISSN: 2377-4304


Research Article Volume 12 Issue 5
Obstetrics and Gynecology, University Hospital of Fuenlabrada, Rey Juan Carlos University, Spain
Correspondence: Natalia Pagola Limón, Obstetrics and Gynecology, University Hospital of Fuenlabrada, Universidad Rey Juan Carlos, Spain, Tel 687967847
Received: October 08, 2021 | Published: October 22, 2021
Citation: Pagola NL, Valle ERV, Rodríguez MH, et al. Maternal and neonatal outcomes in prolonged second stage deliveries in nulliparous. Obstet Gynecol Int J. 2021;12(5):323-329. DOI: 10.15406/ogij.2021.12.00601
Introduction: The prolongation of the second stage of labor in pregnant women, in order to reduce the rate of cesarean sections, constitutes a scientific and clinical dilemma. This controversy is generated because the increase in the prolonged second stage time can increase the maternal and neonatal risks.
Objective: To analyze differences in maternal and neonatal outcomes between pregnant women who have a prolonged vs non-prolonged delivery. To study those pregnant women who have prolonged second stage (>180 minutes) and identify differences between them according to mode of delivery (non-operative, operative or cesarean delivery).
Material and methods: Prospective cohort study of all nulliparous pregnant women treated at the Hospital Universitario de Fuenlabrada between January 1, 2018 and December 31, 2019. Differences in pregnant women with prolonged versus non-prolonged delivery are analyzed. Those cases in which the prolonged second stage period was equal to or greater than 180 minutes were selected and differences according to the mode of delivery were studied. During the study period, 944 women met the inclusion criteria, of which 445 (47.1%) had prolonged second stage periods equal to or greater than 180 minutes.
Results: Prolonged second stage is associated with a higher rate of operative delivery 44.5% vs. 28.1% and a higher rate of cesarean section 6.7% vs. 2% (p: 0.000), a higher rate of shoulder dystocia 3.8% vs. 1.6%, greater weight at birth of the newborn 3279 g vs 3119 g and greater perinatal trauma 13.3 vs 6.6% compared with non-prolonged second stage delivery.
By selecting only pregnant women with prolonged delivery, we observed a higher rate of complications of surgical wound in caesarean sections 13.3%, vs 1.5% in operative delivery and 0% in spontaneous vaginal delivery and a higher rate of grade III-IV degree perineal lacerations in deliveries eutocic and instrumental.
With respect to the neonate, a greater weight of the newborn is observed in caesarean sections 3445 grams compared to eutocic deliveries 3230 grams and operative delivery 3275 grams (p: 0.001), a higher rate of type III resuscitation in those neonates born by caesarean section 26, 7% vs 4.2% in spontaneous vaginal delivery and 5.6% in operative delivery and a higher rate of admission to the neonatal ICU in caesarean sections 26.7% vs 6.9% spontaneous vaginal delivery and 9.1% operative delivery (p: 0.002) .
Conclusion: A higher rate of operative delivery and cesarean sections has been observed in pregnant women with prolonged second stage, as well as a higher rate of shoulder dystocia, newborn weight, and perinatal trauma compared with non-prolonged delivery.
When studying the cohort of pregnant women with prolonged second stage, there is a higher rate of cesarean section in pregnant women with a previous suspicion of fetal macrosomia, a higher weight of the newborn at birth, a higher rate of type III neonatal resuscitation and admission of the newborn to the neonatal ICU in pregnant women. that end in caesarean section with respect to spontaneous vaginal delivery or operative delivery.
The length of the second stage of labor or the second stage of labor has been subject to controversy for the last 200 years. The death of Princess Charlotte, her fetus at term (the future King of England), and the subsequent suicide of her obstetrician (the famous case of the triple obstetric tragedy) in 1821 after 24 hours of second stage, highlighted the importance to put a time limit on that second stage period.1
The maximum 2-hour second stage limit in nulliparous women was described in the US at the beginning of the 20th century2 when J. Whitridge Williams3 observed that time intervals greater than 2 hours were harmful for the mother and the neonate.
In the following years, DeLee popularized the use of prophylactic forceps to end the second stage of labor within 2 hours of full dilation.4 The advantages of this prophylactic forceps were the protection of the maternal and neonatal perineum.
In 1952, Hellman and Prystowsky published a study in which> 13,000 deliveries were observed at Johns Hopkins Hospital in Baltimore, observing an increase in infant mortality above 2.5 hours after delivery.5
In the 21st century, improvements in the field of obstetrics, intrapartum monitoring, greater follow-up during pregnancy, greater safety of tocurgia have significantly decreased maternal-fetal morbidity and mortality, but there has been a trend to increase in the rate of caesarean sections, which continues to increase day by day without clear benefits, which has made the Gynecology and Obstetrics societies have met and agreed on guidelines to reduce the rate of caesarean sections safely. ACOG published in 2014 a consensus document entitled “Safe Prevention of the Primary Cesarean Delivery”6 which is highly influenced by the NICHD workshop published as “Preventing the first cesarean delivery”.7
The conclusions of these consensus documents redefine the hours of delivery in nulliparous and multiparous pregnant women with and without epidural and consider second stage of labor or delivery stopped in >4 hours for nulliparous women with epidural, >3 hours for nulliparous women without epidurals, >3 hours for multiparous women with epidural and >2 hours for multiparas without epidural (Figure 1).
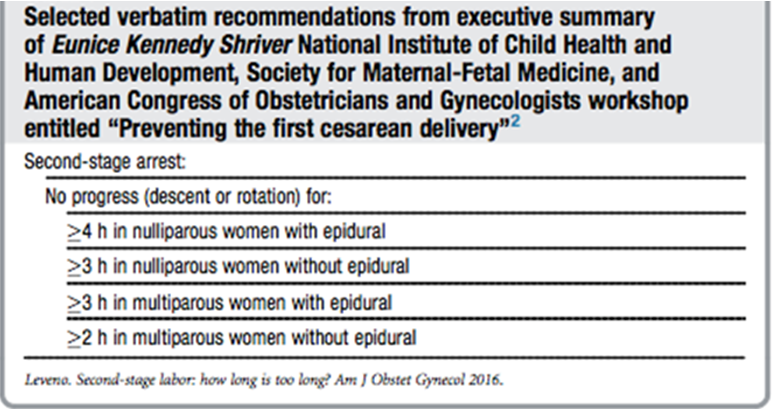
Figure 1 Leveno K (2016). Second-stage labor: how long is too long?2
Regardless of these “new times”, professional guides define the term “prolonged prolonged second stage ” or “Prolonged Second Stage of Labor” (PSSL) to> 3 hours for nulliparous with epidural,> 2 hours for nulliparous without epidural,> 2 hours for multiparous women with epidural and> 1 hour for multiparous women without epidural.
A justification for these new second stage times that some authors consider arbitrary is based on a study by Zhang et al, which found that the 95th percentile of time to second stage of labor for nulliparous women with epidural is 3.6 hours.8 Or in a retrospective study published by Cheng et al in 2011 in which they compared perinatal results of nulliparous women who underwent an operative delivery before 3 hours of delivery vs vaginal delivery after more than 3 hours of delivery, they have lower rates III and IV grade degree perineal lacerations (aOR 0.63, 95% CI 0.51–0.77), neonatal cephalohematoma (aOR 0.48, 95% CI 0.28–0.83) and admissions to neonatal ICU (aOR 0.70, 95% CI 0.49–0.99) compared to patients to which the delivery is instrumented before 3 hours.9
Delay of targeted bids vs active bids
Several studies have focused on the importance of delaying pushing (waiting 1-3 hours to start active pushing) as an important factor affecting the second stage of labor. Data from a meta-analysis of 12 randomized controlled clinical trials show that in term pregnant women, with a single pregnancy, a fetus in cephalic and epidural anesthesia, delaying active pushing is associated with an increased incidence of spontaneous vaginal delivery and a similar rate of operative delivery and caesarean section compared with early active pushing. The duration of the delivery is longer, the duration of the directed pushing is similar, and there are no differences in maternal-fetal outcomes.10,11
In Spain, in 2010, the Ministry of Health, Consumption and Social Welfare published a consensus document "CLINICAL PRACTICE GUIDE ON NORMAL LABOR CARE" published by a multidisciplinary team and agreed with the Spanish Society of Gynecology and Obstetrics where it recommends in women with neuraxial analgesia, direct the pushes once the passive phase (2 hours in both nulliparous and multiparous women) of the second stage of labor has been completed, based on the Nice Guide and on several studies that conclude that the total duration of the second stage is significantly longer when pushing is delayed, but with a shorter duration of the active push. In addition, there is a lower risk of medium forceps deliveries and rotational operative delivery when pushing is delayed.
Objectives
Prospective cohort study of all women treated at the Hospital Universitario de Fuenlabrada between January 1, 2018 and December 31, 2019 who met the following inclusion criteria: term gestation (37 or more gestational weeks), absence of previous deliveries or cesarean sections, having reached full dilation.
The variables analyzed are maternal age, gestational age, BMI, geographic origin, duration of second stage, previous suspicion of macrosomia, mode of delivery, mode of delivery, indication for instrumental/cesarean delivery, type of instruments, epidural anesthesia, shoulder dystocia, complications in the puerperium, neonatal weight, Apgar minute 1, Apgar minute 5, cord pH, type of resuscitation, admission of the newborn to the neonatal ICU and neonatal trauma.
The sample is divided between pregnant women with prolonged versus non-prolonged delivery to analyze significant differences.
Those cases in which the prolonged second stage period was equal to or greater than 180 minutes were selected and differences were analyzed by mode of delivery: eutocic, instrumental or caesarean section.
Categorical variables are defined according to their frequency distribution, continuous variables according to their mean and standard deviation or median and interquartile range. Comparisons between groups are made with the Chi-square test, ANOVA or the Kruskal Wallis test.
During the study period, 944 women met the inclusion criteria, of which 445 (47.1%) had prolonged second stage periods equal to or greater than 180 minutes.
The variables studied for all pregnant women included in the study are shown in the Table 1. It should be noted that although in our Hospital, we follow the Ministry's guidelines that recommend delaying active pushing for 2 hours in nulliparous women with epidurals, the mean delivery time is 172 minutes and only 47% of pregnant women have prolonged delivery (> 180 minutes), either because the delivery progresses favorably and the pregnant woman cannot avoid her feeling of push, or because of alterations in the electronic fetal monitoring that make it necessary to start the directed push to advance the delivery earlier (Figure 2).
|
Variable |
Distribution (N = 944) |
|
|
Maternal age |
30.9 (5.5) |
|
|
Gestational age |
39.9 (1.2) |
|
|
BMI (Kg / m2) * |
24.2 (4.9) |
|
|
Second stage time (minutes) |
172.1 (93.8 - 217.7) |
|
|
Second stage> 180 minutes |
445 (47.1) |
|
|
Second stage <180 minutes |
499 (52.9) |
|
|
Geographical origin |
Caucasian |
765 (81.5) |
|
Sub-Saharan |
29 (3.1) |
|
|
Asian |
9 (1.0) |
|
|
Latin American |
69 (7.4) |
|
|
Maghreb |
57 (7.1) |
|
|
Suspicion of macrosomia |
59 (6.6) |
|
|
Delivery type |
Spontaneous |
447 (47.4) |
|
Induced |
497 (52.7) |
|
|
Mode of delivery |
Spontaneous |
566 (60.0) |
|
Instrumental |
338 (35.8) |
|
|
Caesarean section |
40 (4.2) |
|
|
Instrument / cesarean indication |
RPBF |
156 (40.8) |
|
Expulsive relief |
190 (49.7) |
|
|
Cephalopelvic disproportion |
36 (9.4) |
|
|
Instrument type |
Kiwi suction cup |
49 (14.5) |
|
Metal suction cup |
143 (42.2) |
|
|
Forceps |
128 (37.8) |
|
|
Spatula |
18 (5.39) |
|
|
Other |
1 (0.3) |
|
|
Epidural anesthesia |
913 (96.7) |
|
|
Episiotomy |
435 (46.3) |
|
|
Shoulder dystocia |
25 (2.7) |
|
|
Complications in the puerperium |
182 (19.3) |
|
|
Apgar in the first minute |
9 (9-9) |
|
|
Apgar in the fifth minute |
10 (10-10) |
|
|
cord pH |
7.2 (0.1) |
|
|
Newborn weight (grams) |
3200 (2910 - 3449.5) |
|
|
Admission to neonatal ICU |
80 (8.5) |
|
|
REA type |
0 |
745 (79.0) |
|
1 |
137 (14.5) |
|
|
2 |
1 (0.1) |
|
|
3 |
60 (6.4) |
|
|
Perinatal trauma |
92 (9.7) |
|
Table 1 The variables studied for all pregnant women included in the study
Other data to highlight are the low rate of cesarean section in these nulliparous pregnant women who reached full dilation (4.2%). Overall maternal complications are 19.3%, although only short-term complications are studied. The rate of admission of the neonate to the ICU is 8.5% and perinatal trauma is 9.7%.
When dividing the sample into those pregnant women with prolonged vs non-prolonged prolonged second stages (Table 2) we can observe significant differences in gestational age, greater in prolonged prolonged second stages 40 vs 39.8 (p: 0.004) and greater use of epidurals in prolonged prolonged second stages 98.7 vs 95 % (p: 0.002).
|
|
Expulsive not prolonged (N = 499) |
Prolonged explosive |
p |
|
|
(N = 445) |
||||
|
Maternal age (years) |
31.1 (26.2 - 34.5) |
31.8 (28.4 - 35.2) |
0.134 |
|
|
Gestational age (weeks) |
39.8 (1.2) |
40.0 (1.1) |
0.004 |
|
|
BMI (Kg / m2) |
23.0 (21.0 - 26.1) |
23.1 (20.7 - 26.9) |
0.663 |
|
|
Origin # |
Caucasian |
392 (78.9) |
373 (84.4) |
0.139 |
|
Sub-Saharan |
19 (3.8) |
10 (2.3) |
||
|
Asian |
5 (1.0) |
4 (0.9) |
||
|
Latin American |
45 (9.1) |
24 (5.4) |
||
|
Maghreb |
36 (7.2) |
31 (7.0) |
||
|
Suspicion macrosomia # |
21 (4.4) |
38 (8.9) |
0.006 |
|
|
Induced labor # |
258 (51.7) |
239 (53.7) |
0.538 |
|
|
Use of epidural # |
474 (95.0) |
439 (98.7) |
0.002 |
|
|
Delivery mode |
Spontaneous vaginal |
349 (69.9) |
217 (48.8) |
0 |
|
Instrumental |
140 (28.1) |
198 (44.5) |
||
|
Caesarean section |
10 (2.0) |
30 (6.7) |
||
|
Shoulder dystocia # |
8 (1.6) |
17 (3.8) |
0.034 |
|
|
Complication |
Hemorrhage |
13 (2.6) |
24 (5.4) |
0.218 |
|
Endometritis |
2 (0.4) |
7 (1.6) |
||
|
Wound complications |
7 (1.4) |
7 (1.6) |
||
|
III-IV degree lacerations |
36 (7.2) |
36 (8.1) |
||
|
Anemia <10 g / dL |
6 (1.2) |
4 (0.9 |
||
|
Ehe |
7 (1.4) |
4 (0.9) |
||
|
Other |
16 (3.2) |
13 (2.3) |
||
|
Birth weight (g) ** |
3119 (420) |
3279 (415) |
0 |
|
|
pH * |
7.22 (7.17 - 7.28) |
7.23 (7.18 - 7. 28) |
0.422 |
|
|
Apgar1 * |
9 (9 - 9) |
9 (9 - 9) |
0.2 |
|
|
Apgar5 * |
10 (10 - 10) |
10 (10 - 10) |
1,000 |
|
|
REA # |
0 |
403 (80.8) |
342 (77.0) |
0.267 |
|
1 |
63 (12.6) |
74 (16.7) |
||
|
2 |
1 (0.2) |
0 (0) |
||
|
3 |
32 (6.4) |
28 (6.3) |
||
|
Admission to ICU # |
39 (7.8) |
41 (9.2) |
0.441 |
|
|
Perinatal Trauma |
33 (6.6) |
59 (13.3) |
0.001 |
|
Table 2 Dividing the sample into those pregnant women with prolonged vs non-prolonged second stage
We obtain more relevant differences in the mode of delivery with a higher rate of operative delivery 44.5% vs 28.1% and a higher rate of cesarean section 6.7% vs 2% (p: 0.000), higher rate of shoulder dystocia 3 , 8% vs 1.6%, higher birth weight of the newborn 3279 g vs 3119 g and greater perinatal trauma 13.3 vs 6.6% in prolonged delivery. In the rest of the variables we have not observed significant differences.
When selecting the cohort of those pregnant women who have had prolonged second stage (Table 3) and dividing them according to mode of delivery, we observed a higher rate of cesarean section 30% vs 7.3% (eutocic) and 7.5% (operative delivery) in those pregnant women with suspected fetal macrosomia prior to delivery. Regarding maternal complications, there are significant differences in surgical wound complications, higher in caesarean sections 13.3%, vs 1.5% and 0% and higher rate of grade III-IV degree perineal lacerations in eutocic and instrumental deliveries, it is striking the highest rate of serious degree perineal lacerations in spontaneous vaginal deliveries 10.6% vs operative delivery 6.6%. (p: 0.000).
|
|
Spontaneous (N = 217) |
Instrumental (N = 198) |
Cesarean section (N = 30) |
p |
||
|
Maternal age |
31.8 (27.9 - 34.9) |
31.5 (28.2 - 34.8) |
34.2 (30.9 - 36.8) |
0.048 |
||
|
Gestational age |
40.1 (39.2 - 40.9) |
40.1 (39.4 - 41.0) |
40.7 (39.3 - 41.1) |
0.41 |
||
|
BMI (Kg / m2) |
23.0 (20.5 - 26.3) |
23.1 (20.7 - 26.8) |
26.1 (21.5 - 28.4) |
0.066 |
||
|
Origin |
Caucasian |
176 (81.5) |
173 (88.3) |
24 (80.0) |
0.063 |
|
|
Sub-Saharan |
8 (3.7) |
1 (0.5) |
1 (3.3) |
|||
|
Asian |
2 (0.9) |
2 (1.0) |
0 (0.0) |
|||
|
Latin American |
18 (8.3) |
5 (2.6) |
1 (3.3) |
|||
|
Maghreb |
12 (5.6) |
15 (7.7) |
4 (13.3) |
|||
|
Suspicion of macrosomia |
15 (7.3) |
14 (7.5) |
9 (30.0) |
0 |
||
|
Induced labor |
116 (53.5) |
101 (51.0) |
22 (73.3) |
0.073 |
||
|
Epidural anesthesia |
212 (97.7) |
197 (99.5) |
30 (100) |
0.228 |
||
|
Shoulder dystocia |
4 (1.8) |
13 (6.6) |
0 (0) |
0.023 |
||
|
Maternal complications |
Postpartum hemorrhage |
8 (3.7) |
14 (7.1) |
2 (6.7) |
0 |
|
|
Endometritis |
6 (2.8) |
1 (0.5) |
0 (0) |
|||
|
Wound complications |
0 |
3 (1.5) |
4 (13.3) |
|||
|
Grade III-IV lacerations |
23 (10.6) |
13 (6.6) |
0 (0) |
|||
|
Anemia <10 g / dL |
1 (0.5) |
3 (1.5) |
0 (0) |
|||
|
Ehe |
2 (0.9) |
2 (1.0) |
0 (0) |
|||
|
Other |
4 (1.8) |
8 (4.0) |
1 (3.3) |
|||
|
Weight RN (grams) |
3230 (2990 - 3460) |
3275 (3018 - 3586) |
3445 (3310- 3820) |
0.001 |
||
|
Apgar first minute |
9 (9 - 9) |
9 (8 - 9) |
9 (7 - 9) |
0.084 |
||
|
Apgar five minutes |
10 (10 - 10) |
10 (10 - 10) |
10 (9 - 10) |
0.002 |
||
|
pH |
7.23 (0.07) |
7.22 (0.08) |
7.24 (0.07) |
0.552 |
||
|
REA type |
0 |
180 (83.0) |
148 (75.1) |
14 (46.7) |
0 |
|
|
1 |
28 (12.9) |
38 (19.3) |
8 (26.7) |
|||
|
2 |
0 (0) |
0 (0) |
0 (0) |
|||
|
3 |
9 (4.2) |
11 (5.6) |
8 (26.7) |
|||
|
Admission to ICU of the NB |
15 (6.9) |
18 (9.1) |
8 (26.7) |
0.002 |
||
|
Perinatal trauma |
Cutaneous |
4 (1.8) |
6 (3.0) |
1 (3.3) |
0.048 |
|
|
Hematoma NDE |
0 (0) |
6 (3.0) |
1 (3.3) |
|||
|
Cephalohematoma |
4 (1.8) |
9 (4.6) |
1 (3.3) |
|||
|
Caput sucedaneum |
11 (1.8) |
11 (5.6) |
3 (10.0) |
|||
|
Cranial fracture |
0 (0) |
1 (0.5) |
0 (0) |
|||
|
Clavicular fracture |
0 (0) |
3 (1.5) |
0 (0) |
|||
|
CNS hemorrhage |
0 (0) |
0 (0) |
1 (3.3) |
|||
|
Facial paralysis |
0 (0) |
2 (1.0) |
0 (0) |
|||
|
|
Brachial palsy |
0 (0) |
1 (0.5) |
0 (0) |
|
|
Table 3 The cohort of those pregnant women who have had prolonged second stage
With respect to the neonate, a greater weight of the newborn is observed in caesarean sections 3445 g with respect to eutocic deliveries 3230 g and operative delivery 3275 g (p: 0.001) and the most clinically relevant is that we have observed a higher rate of type III resuscitation in those neonates born by cesarean section 26.7% vs 4.2% in spontaneous vaginal delivery and 5.6% in operative delivery and a higher rate of admission to the neonatal ICU in cesarean sections 26.7% vs spontaneous vaginal delivery 6.9% and operative delivery 9 , 1% (p: 0.002). Regarding perinatal trauma, although we observed significant differences by mode of delivery route (p: 0.045), since the number of trauma cases was so small, it was not clinically relevant.
The prolongation of the second stage of labor in pregnant women, in order to reduce the rate of cesarean sections, constitutes a scientific and clinical dilemma. This controversy is generated because the increase in the prolonged second stage time can increase the maternal and neonatal risks. When conducting a review of the literature, we found very disparate results.12
Sthephansson et al.13 carry out a retrospective descriptive study with a large sample size and conclude that the rate of complications increases according to the hours of delivery.
Grobman et al.14 also carry out an observational study and state that a longer duration of active pushing time is associated with an increased relative risk, but with a small absolute difference in the risk of neonatal complications. About 78% of women have vaginal deliveries even after 4 hours of active pushing.
Gimovsky et al.15–17 carry out a bibliographic review and conclude that around 80.2% of nulliparas with epidurals and prolonged second stage of labor end in vaginal delivery.
The only randomized clinical trial published by Berghella et al.18 found that extending the duration of the second stage of labor reduces
the incidence of cesarean sections by a significant percentage (55%) without increasing risks for either the mother or the baby neonate.
Finally, the observational study by Zipori et al.19 again shows that the new policy promoted by ACOG of increasing the duration of the second stage of labor significantly reduces the rate of cesarean sections in both nulliparous and multiparous women. Although this practice of extending the delivery is also associated with a slight increase in instrumental vaginal delivery in nulliparous women and other short-term maternal complications such as early postpartum hemorrhage and 3rd and 4th degree degree perineal lacerations. Regarding neonatal outcomes, a higher incidence of cord pH has been
observed 7 in the second period, but without implications in early neonatal neurological involvement.
This review of the literature, aims that the scientific evidence in which base is scarce, based on studies with little statistical power and many limitations as to establish relevant results, so the prolonged second stage times that they changed according to the ACOG and that we have followed since then in almost all delivery rooms in our country and the rest of the first world, they are based on arbitrary times, chosen on the basis of poor quality studies.
Despite this, the obstetricians who work day by day in the delivery rooms do believe that increasing the duration of delivery has been clearly effective in reducing the rate of cesarean sections, increasing the rates of spontaneous vaginal birth or allowing operative deliveries much less aggressive than those we perfomed years ago, when we intervened in the first two hours of full dilation.
The slight increase in maternal complications reported in some of these studies is based on short-term complications, such as early postpartum hemorrhage, although none of the studies report serious consequences of these hemorrhages. It is evident that if we do fewer caesarean sections, we will implement more deliveries, and this leads to a higher rate of perineal pathology, but none of these studies detail long-term consequences of these degree perineal lacerations.
When analyzing the neonatal consequences, we have found varied results, it seems that there is a slight tendency to worse results in the short term, such as lower cord pH, or greater admissions to the ICU, but in no study was it observed that these results have neurological consequences for the long-term neonate.
Our study, being an observational study, and taking into account that our hospital works respecting no active pushing hours in the second stage, pregnant women who have prolonged second stage periods of less than 180 minutes are usually pregnant with deliveries that evolve very favorably with greater tendency to spontaneous vaginal delivery compared to patients with longer prolonged second stage deliveries and longer time of active pushing, which is normal to be associated with more dystocic deliveries and therefore we do observe a higher rate of cesarean section and operative delivery in pregnant women with prolonged delivery, but as strength, when studying those pregnant women with prolonged second stage, we did observe significant worse results for both the mother and the newborn in those deliveries with prolonged delivery that end in cesarean section.
It is clear that in order to obtain more illuminating results than those published to date, randomized clinical trials should be carried out with a much larger recruited population, randomizing into 2 groups according to old guidelines vs. current guidelines for second stage times, stratifying according to the number of passive prolonged second stage hours. respected, and objectifying results of the rate of cesarean section, operative delivery and spontaneous delivery, also analyzing short-term maternal and neonatal results, but above all, emphasizing long-term consequences, mainly in pelvic floor pathology in the mother and neurological and psychomotor development in the first years of the newborn's life.
A higher rate of operative delivery and cesarean sections has been observed in pregnant women with prolonged delivery, as well as a higher rate of shoulder dystocia, newborn weight, and perinatal trauma compared with non-prolonged delivery.
When studying the cohort of pregnant women with prolonged delivery, there is a higher rate of cesarean section in pregnant women with a previous suspicion of fetal macrosomia, a higher weight of the newborn at birth, a higher rate of type III neonatal resuscitation and admission of the newborn to the neonatal ICU in pregnant women. That end in cesarean section with respect to spontaneous vaginal delivery or operative delivery.
None.
None.
The authors did not report any potential conflicts of interest.

©2021 Pagola, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.