eISSN: 2377-4304


Research Article Volume 13 Issue 3
1Section of Fetal Therapy and Fetal Surgery Unit, Division of Maternal Fetal Medicine, Department of Obstetrics and Gynecology Hospital de San José and Department of Obstetrics and Gynecology Fundación Universitaria de Ciencias de la Salud – FUCS, Colombia
2Section of Fetal Therapy and Fetal Surgery Unit, Division of Maternal-Fetal Medicine, Department of Obstetrics and Gynecology, Clínica Colsubsidio 94, Bogotá, Colombia
3Departament of Radiology and Diagnostic images, Clínica de la Mujer- Grupo Quironsalud, Bogotá, Colombia
4Fetal Therapy and Surgery Network - FetoNetwork Colombia
5Department of Obstetrics and Gynecology, Faculty of Medicine, Universidad Nacional de Colombia, Bogotá, Colombia
Correspondence: Saulo Molina Giraldo MD, MSc, PHD(e), Maternal Fetal Medicine Unit, Therapy, Fetoscopic and Fetal Surgery Center. Clínica de la Mujer-Grupo Quironsalud, Bogotá, Carrera 19C #90-30, 4th floor, Colombia, Tel +573102128382
Received: April 25, 2022 | Published: May 06, 2022
Citation: DOI: 10.15406/ogij.2022.13.00640
Introduction: The prognosis in fetal lung disease is related to the size of the pulmonary malformation and secondary pulmonary hypoplasia. The mass effect on the underlying fetal lung results in a decrease in fetal lung volume and an increased likelihood of developing respiratory distress during the neonatal period.
Objectives: Estimate the lung volume cut-off points related to neonatal morbidity and mortality in fetuses with congenital pulmonary malformation measured through magnetic resonance imaging.
Methodology: Analytical retrospective cohort study from July 1, 2013, to June 30, 2017. Lung volumes were measured by magnetic resonance imaging in fetuses with congenital pulmonary malformation. The different measures are described and the association of lung volume with neonatal mortality is evaluated.
Results: We analyzed 26 fetuses with congenital pulmonary malformation. The mortality described was 46.1% (12/26). The mean lung volume in the group with mortality was 19.7cm3 (95% CI 12.1-27.3), vs 58.6cm3 in the group without mortality (95% CI 39.0-78.1) (p=0.0010). Average lung volumes less than 34.9 cm3 were associated with higher mortality.
Conclusion: The perinatal result of fetal lung disease is related to lung volume measured with Fetal Magnetic Resonance Imaging, finding that lung volumes less than 34.9cm3 were associated with higher mortality.
Keywords: pulmonary diseases, lung volume measurements, magnetic resonance imaging, perinatal mortality
Congenital thoracic and pulmonary malformations are a heterogeneous group of diseases that have an important influence on childhood morbidity and mortality.1 Among the pulmonary malformations in fetuses we found congenital diaphragmatic hernia (CDH), congenital cystic adenomatoid malformation (CCAM), bronchopulmonary sequestration (BPS), congenital lobar emphysema, mediastinal teratoma, among others.2 It has been reported that, in general, the prognosis depends directly on the size of the lung mass, on the secondary physiological changes generated by its effect on the fetal anatomy, and on mediastinal deviation, circulatory collapse, and the development of Hidrops fetalis as well.3 Most deaths occur secondary to pulmonary hypoplasia or are associated with pulmonary hypertension in the neonatal period. The prognosis worsens when it is associated with other congenital abnormalities and chromosomal abnormalities detected in the karyotype.4
The prenatal diagnosis of these diseases is a fundamental tool to offer timely treatment and reduce perinatal morbidity and mortality.1 The widespread use of prenatal ultrasound is sensitive for diagnosis but it has low specificity.5 On the other hand, fetal magnetic resonance imaging (fMRI) improves the evaluation of the lung anatomy, it can help confirming or ruling out the diagnostic suspicion made by ultrasound. It provides complementary information for genetic counseling, and supports the obstetric decision.6,7 In addition, fMRI adds to ultrasound the possibility of differentiating the types of congenital lung lesions8 and it seems to be less limited due to maternal obesity, oligohydramnios, and the fetal rib cage compared to ultrasound;9 Additionally, obtaining multiple slices every 3 to 5 mm it can be performed, in a post-process study, the calculation of the individual or global lung volume.10
In the fetus, pulmonary compression of any origin is associated with hypoplasia and neonatal respiratory distress; the earlier and more severe the compression, the worse the prognosis. This pulmonary hypoplasia implies a decrease in lung volume.11 The measurement of lung volumes by fMRI would predict the degree of pulmonary involvement, establishing the prognosis and improving the strategies to be used in the medical team of newborn care.10 In recent years, some studies have been published that relate lung volumes measured by magnetic resonance imaging with fetal prognosis, mainly in fetuses with a congenital diaphragmatic hernia. However, there is no specific cut-off point that is related to neonatal morbidity and mortality.
This research explores the association between lung volumes measured by magnetic resonance imaging in fetuses with a diagnosis of pulmonary malformation and neonatal morbidity and mortality.
We carried out a retrospective cohort study in 2 Maternal-Fetal Medicine Units in Bogotá - Colombia. In addition, we conducted a retrospective review of the clinical history of patients with a diagnosis of fetal pulmonary malformation by ultrasound and magnetic resonance imaging performed between weeks 18 and 32 of gestation. Patients who had fMRI that could not be analyzed post-process, who had another fetal malformation associated with mortality, anhydramnios, or who had no follow-up recorded in the medical history were excluded.
Data collection was carried out independently. A data collection form was filled out for each case, including sociodemographic data, obstetric and medical history, perinatal results (including main causes of perinatal morbidity and mortality).
The variables included were: mother's age, parity, number of prenatal check-ups, delivery route, gestational age at birth, birth weight, length at birth, sex, type of lung malformation, lung volumes (right, left, and average), newborn mortality, time of death, neonatal complications and total length of stay in the Neonatal Intensive Care Unit.
The different lung volumes were considered as the exposure variable. The primary outcome was associated with neonatal mortality.
The fetal lung volume was measured using fMRI, which was performed between 24-32 weeks of gestation (Figure 1). Medical records of the patients who met the inclusion criteria and who belonged to the participating Maternal-Fetal Medicine Units were selected. We evaluated the fMRI using CDs with information extracted in DICOM -Digital Imaging and Communication On Medicine, a standard protocol for the transmission of medical images and data between medical-purpose hardware-. We visualized and analyzed the information through the Horos medical image viewer, open-source based on the OsiriXTM application, available under the GNU Lesser General Public License, Version 3 (LGPL-3.0), with which we elaborated a structured report focused on the fetal thorax. The radiology specialist who measured the lung volumes was unaware of the neonatal results or the complications that the newborns presented to control biases.
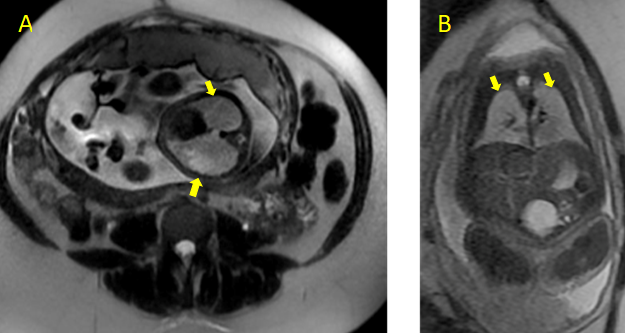
Figure 1 Acquisitions in T2 sequences, A. axial image in 4-chamber sections, B. coronal image of the lung parenchyma. Arrows shows fetal lungs.
We evaluated images covering the entire thorax, from the area of regions of interest following the pulmonary limits in consecutive images multiplied by the thickness of the section. In addition, we made independent measurements of the right and left lungs and the calculation of the average volume as well. The formula used for this calculation was: height x width x thickness of the cut, adding the total of cuts for each lung.
The data entry was carried out in a specific database in a Microsoft Excel - Office 2013 spreadsheet.
We carried out a descriptive analysis of the information. The quantitative variables were summarized by arithmetic mean or median, according to their distribution. To assess the normality of the data, the Shapiro-Wilk test was used. The qualitative variables were analyzed in absolute and relative frequencies. For the comparison of means, the student's t-test was used, in the case of medians, non-parametric tests were used. Using as dependent variable the final result of death or perinatal morbidity (Yes vs. No), its association with the independent variables investigated was evaluated, using a chi-square test.
Finally, we calculated the cut-off point that allows identifying the mortality of the participants with lung volume using a ROC Curve.
During the study period, 89 fetuses presented a diagnosis of fetal lung malformation and, 33 of them had a report of magnetic resonance imaging. Information on the delivery and evolution of the newborn was not available in 7 of the cases. A total of 26 fetuses met the inclusion criteria and were included for the final data analysis.
The age of the mother at the time of diagnosis was 26 (19-37) years, the majority were between the first and second gestation (Table 1).
|
Characteristic |
n=26 |
Maternal |
|
|
Age |
26 ± 3 yrs |
|
Parity |
||
1 Pregnancy |
14 (53,8 %) |
|
2 Pregnancies |
10 (38,5%) |
|
3 o + Pregnancies |
2 (7,7%) |
|
Neonatal |
||
Gestational age |
38 wks ± 5 d |
|
Weight |
2790 grs ± 380 grs |
|
APGAR per minute |
||
< 3 |
7 (26,9%) |
|
≥ 3 |
19 (73,1%) |
|
APGAR at 5 minutes |
||
< 7 |
10 (38,4%) |
|
≥ 7 |
16 (61,6%) |
|
NICU stay |
6 (2-10 range ) |
|
Delivery type |
||
EXIT |
12 (46,2%) |
|
Caesarean section |
10 (38.5%) |
|
Vaginal |
4 (15,3%) |
|
Data represent median ± SD or n% |
||
Table 1 Maternal and neonatal characteristics
At the time of delivery, the median gestational age was 38 weeks. The minimum gestational age at birth was 29 weeks. 73% of the newborns were full term; 34.6% had low birth weight (<2500grams), with a mean weight of 2790 grams and a median height of 48 centimeters.
The APGAR score at one minute had a median score of 5, finding that 26.9% of the newborns had a score lower than 3; at five minutes with a median score of 7. 38.4% of the population presented APGAR <7. 46.1% of the cases were taken to EXIT, 38.5% had a cesarean delivery and 15.4% were delivered vaginally.
When we were analyzing the distribution by type of malformation, we found that 50% of the population studied had a diaphragmatic hernia, in the second place in frequency, we found 38.46%, the CCAM II-III. There was a case of bronchopulmonary sequestration corresponding to 3.85%, a case of a hybrid mass, and a case of unilateral pulmonary agenesis.
Regarding the location of the lesion, no bilateral lesions were found in the analyzed population. The lung most frequently affected was the left with 73.1% compared to the right (26.9%).
The most frequent neonatal complications were pulmonary hypertension in 34.6% of cases and cardiogenic shock in 26.9% of cases. In the other hand, 15.4% of secondary complications non-related to prematurity was recorded, and one case of neonatal sepsis and one case of postoperative sepsis.
The mean stay in the NICU was 6 days for the survivors and there was no statistically significant difference about the cause of admission and the stay in the NICU. One case of prolonged hospitalization (25 days) for postoperative sepsis was reported. The mortality recorded was 46.2% of the cases and 100% occurred in the first 48 hours of the neonatal period. The highest mortality (83.3%) was found in neonates with a diaphragmatic hernia, while for another type of injury it was 8.3% (p 0.01). For neonates with CCAM II-III, survival was 65%. Mortality in left lesions was 52.6% and in right lesions 28.6%, however, the differences are not statistically significant.
We found a significant decreased in the lung volume in deceased neonates (Table 2). The average lung volume in the group that presented mortality was 19.7cm3 (95% CI 12.1-27.3), while the group without mortality presented an average lung volume of 58.6 cm3 (95% CI 39, 0-78.1) with a statistically significant difference (p=0.0010).
Mortality |
Right lung volume* |
Left lung volume* |
Bilateral lung volume* |
No |
30,04 (IC 95 % 20,4 – 39,6) |
28,5 (IC 95% 17,3 – 39,7) |
58,6 (IC 95% 39,0 – 78,1) |
Yes |
13,7 (IC 95 % 8,5 – 19) |
5,9 (IC 95% 0.94 – 10,9) |
19,7 (IC 95% 12,1 – 27,3) |
Table 2 Mortality relationship with lung volumes (Average and 95% confidence intervals)
The mean for the right lung volume found was 30cm3 (95% CI 20.4-39.6) in the group of patients who survived, while in the deceased it was 13cm3 (95% CI 8.5-19) (p=0.0053).
For left lung volume, comparing survivors with deceased, the mean was 28.5 cm3 (95% CI 17.3-39.7) and 5.9cm3 (95% CI 0.94-10.9) respectively (p=0.0009).
No statistically significant differences were found in neonatal complications according to fetal lung volume.
Using the ROC curve, it was evidenced that average lung volumes less than 34.9cm3 presented mortality of 56.1% (Figure 2) with a sensitivity of 83.33% and a specificity of 78.57% to predict mortality.
Today's prenatal diagnostic tools allow the reliable characterization of different lesions in fetuses. However, they are not always related to the prognosis of the injury; therefore, the identification of prognostic factors that allow considering management in fetal and neonatal life becomes imperative. Pulmonary malformations diagnosed in the prenatal period can be detected through detailed ultrasound and characterized by magnetic resonance imaging, defining with these two diagnostic methods the prognostic factors and associated malformations present in other systems. Magnetic resonance imaging also allows characterization of the lesion with measurement of lung volumes in a more precise way.
The prospective study published by Rypens et al. in 2001, presents a representative group of patients collected over 3 years, in which they described the lung volumes by magnetic resonance imaging without establishing a cut-off point in lung lesions that is related to neonatal prognosis. This work highlights the progressive increase in lung volumes related to gestational age. In the cases of pulmonary pathology, it mentions normal values in the cases of CCAM and the lowest values in cases of diaphragmatic hernia, which could not be established in our study due to the size of the sample.10 More recently, Meyers et al. complemented the work of Rypens by identifying normal lung volumes by magnetic resonance imaging in fetuses between 19 and 22 weeks, without describing critical cut-off points concerning fetal prognosis.12
In fetal medicine, fMRI has shown promising results in the prediction of pulmonary hypoplasia. The use of rapid T2 imaging techniques results in a high-quality evaluation of lung imaging.13,14 It has been previously described that the total lung volume adjusted for fetal weight is significantly lower in fetuses with pulmonary hypoplasia.13–15 Magnetic resonance imaging has also been reported to be more useful as a prognostic indicator in the context of pulmonary hypoplasia secondary to diaphragmatic hernia.15 Our study, in addition to characterizing lesions, raises a cut-off point for lung volume related to neonatal mortality.
In our study, we identified that the most frequent pulmonary malformation was diaphragmatic hernia (50%) and of this, it was mostly located on the left. An average lung volume cut-off point of 34.9 cm3 related to survival was determined in 43.94% regardless of the type of lung malformation; Likewise, an average lung volume of 19.7cm3 was found related to mortality (21.21% of all deaths in patients with an average lung volume lower than this value and 58.33% of all deaths).
In diaphragmatic hernia, the use of the observed/expected lung volume (O E) relationship seems to have a good predictive capacity for adverse perinatal outcomes.16,17 Hidaka et al. studied the ability to predict postnatal outcomes in fetuses with a diaphragmatic hernia by measuring the volume of the right lung by MRI. They evaluated the relationship of the right lung volume by resonance with the fetal weight estimated by ultrasound (VPD/PFE) and the relationship of lung volume O/E, they reported that all fetuses with VPD/PFE <2.8mm3 died, as well as all those with VPD O/E <16.3%.16 Mahieu-Caputo et al. They measured lung volumes O/E and also reported a decrease in fetuses with a diaphragmatic hernia that died.17
Ruano et al.18 retrospectively observed the resonance and ultrasound characteristics of lung volumes and percentage of liver herniation in 80 fetuses with isolated diaphragmatic hernia. In this study, they had an overall mortality of 22.5% and the need for ECMO in 37.2% of the cases. They consider that fetal MRI can reliably predict mortality and the need for ECMO in these fetuses using the combination of PV O / E and the percentage of liver herniation.18
In other types of lung lesions, the literature is scarcer, however, in 2018 Shirota et al.19 published a retrospective analysis of fetuses with congenital airway malformation that required emergency surgery in the neonatal period. They reported in the prenatal MRI analysis that these fetuses had statistically significant differences in the volume of the contralateral lung compared to those that did not require emergency surgery (0.166 ml vs 0.195 ml. P: 0.0188).19
According to our bibliographic search, this is the first work carried out in Latin America that seeks to establish the relationship of lung volumes and morbidity and mortality of newborns affected with pulmonary malformations. The advantage of the study is that it was carried out in two Maternal-Fetal Medicine Units in IV level of care hospitals. Both the ultrasound diagnosis and the post-process evaluation of the magnetic resonance were carried out by expert medical specialists. Although the calculation of lung volumes was performed by a single observer without being able to estimate inter-observer variability, it has the advantage that this radiology specialist is an expert in reading and analysis of fetal magnetic resonance imaging. Subgroup analysis could not be performed due to the size of the sample, since as it was a retrospective study, some data were not included within the variables in the medical records.
By establishing a value of the average lung volume related to survival and mortality in fetal lung injury, we can open a way to establish, as a proposal for a good prognostic factor, a cut-off point of average lung volume related to the value found in the newborns who survived for a population that has the same demographic characteristics. This allows us, in clinical practice and with other prognostic factors, to provide better advice to parents regarding the therapeutic possibilities and neonatal prognosis and also prepare the multidisciplinary team in prenatal care and neonatal in therapeutic possibilities. It is proposed to carry out a prospective and multicenter study that allows to include a greater number of patients who can meet clear inclusion criteria without presenting biases in the information when collecting the data, as well as it would allow having a larger sample of the affected population with different demographic characteristics and thus be able to establish a standard cut-off point that can be applied in populations other than ours. Knowledge of the values of lung volumes associated with neonatal morbidity and mortality will allow not only providing better advice to the family regarding fetal prognosis but also allowing the multidisciplinary team in charge of the care of fetuses with malformations to optimize resources, seeking therapeutic options for decrease pulmonary hypoplasia and impact the perinatal outcome.
The use of magnetic resonance imaging to measure average lung volume seems to be a useful tool to determine fetal prognosis that allows adequate counseling to the family, considering that an average lung volume of 34.9 cm3 has been related to a survival rate of 43.94% regardless of the type of pulmonary malformation; Likewise, an average lung volume of 19.7 cm3 has a strong relationship with postnatal mortality (58.33% of all deaths).
The study was approved by the ethics and research committee of the participating institutions.
None.
Authors declare that there is no conflict of interest.

©2022 , et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.